Today is Dam Proud Day, the annual day of giving for Oregon State University.
You can help sustain the Micronutrient Information Center by making a gift of $5 or more today!
April 24 is Dam Proud Day, our annual day of giving. Support the Linus Pauling Institute with a donation on this day and help us unlock over $60,000 of challenge gifts!
Learn more on our Dam Proud Day website
Contents
See the Skin Health Overview article
In a series of studies beginning in 1929, George and Mildred Burr determined the essentiality of certain fatty acids by feeding rats diets entirely devoid of fat (1, 2). Fat-deprived rats developed visible skin abnormalities, increased water loss across their skin (also referred to as transepidermal water loss (TEWL)), stunted growth, and impaired reproduction. By systematically introducing oils with defined fatty acid combinations in rescue diets, it was determined that oils rich in certain polyunsaturated fatty acids (corn oil, linseed oil) could completely reverse the skin defects in the deficient animals, while oils containing only saturated fatty acids (coconut oil, butter) were ineffectual. Similarly, essential fatty acid deficiency (EFAD) in humans clinically manifests as dermatitis (scaling and dryness of the skin) and increased TEWL (3, 4). The skin abnormalities associated with EFAD have prompted scientists to investigate the effect of essential fatty acid (EFA) supplementation, both topically and through diet, on skin health.
EFAs are a type of polyunsaturated fatty acid (PUFA) that cannot be synthesized in our bodies and must therefore be obtained from the diet. EFAs have documented roles in both the dermal and epidermal layers of the skin, and the appearance of skin is linked to its functional health. There are two classes of EFAs: omega-6 (n-6) and omega-3 (n-3) fatty acids. Linoleic Acid (LA) is the parent compound of the n-6 PUFAs; α-linolenic acid (ALA) is the parent compound of n-3 PUFAs. From these two parent compounds, the body synthesizes longer chain derivatives that also have important functions in healthy skin.
| Fatty acids | Omega-6 PUFA | Linoleic acid | LA |
| γ-Linolenic acid | GLA | ||
| Dihomo-γ-linolenic acid | DGLA | ||
| Arachidonic acid | AA | ||
| Omega-3 PUFAs | α-Linolenic acid | ALA | |
| Eicosatetraenoic acid | ETA | ||
| Eicosapentaenoic acid | EPA | ||
| Docosahexaenoic acid | DHA | ||
| Eicosanoids | Hydroxy fatty acids | 13-hydroxyoctadecadienoic acid | 13-HODE |
| 12-hydroxyeicosatetraenoic acid | 12-HETE | ||
| 15-hydroxyeicosatrienoic acid | 15-HETrE | ||
| 15-hyrdoxyeicosatetraenoic acid | 15-HETE | ||
| 15-hydroxyeicosapentaenoic acid | 15-HEPE | ||
| 17-hydroxydocosahexaenoic acid | 17-HoDHE | ||
| Prostaglandins | Prostaglandin E2 | PGE2 | |
| Prostaglandin E3 | PGE3 | ||
| Enzymes | Cyclooxygenase | COX | |
| Lipoxygenase | LOX | ||
| Phospholipase A2 | PLA2 | ||
The skin is organized into two main layers, the epidermis and the dermis, each comprised of specialized cell types that contribute to the unique properties of the layer. The epidermis is composed of keratinocytes in varying states of differentiation and primarily serves a barrier function, preventing water loss and invasion by microbes and toxins. The main function of the dermis, which consists mostly of collagen and elastin, is to provide physical and nutritional support to the epidermis (5) (see the article on Micronutrients and Skin Health).
The epidermis itself is organized into layers with distinct cell types and lipid composition (6). In the lower layers of the epidermis, keratinocytes divide, differentiate, and are metabolically active. Here, EFAs are incorporated into epidermal phospholipids in the plasma membranes of keratinocytes and membranous organelles (7). The stratum corneum (SC), the uppermost layer of the epidermis, is comprised of terminally differentiated keratinocytes, called corneocytes, encased in a protein and lipid matrix; it is this extracellular lipid matrix that provides the barrier functions of skin (see Figure 1 in the article on Micronutrients and Skin Health). Differentiating keratinocytes deliver barrier lipid to the SC by way of a membrane-bound secretory organelle called a lamellar body (LB). LBs contain a mixture of lipids, which are extruded from the LB and arranged into sheets (lamellae) that encase the corneocytes of the SC (7, 8).
Linoleic acid (LA), the most abundant PUFA present in the epidermis (7, 9, 10), is selectively inserted into two lipid compounds in the SC: acylglucosylceramide and acylceramide (7, 11, 12). Ceramides are a special type of lipid known as a sphingolipid, consisting of a sphingosine backbone with fatty acid attachments; ceramides comprise 40 to 50% of the lipids in the SC (7). The presence of LA in SC ceramides directly correlates with permeability barrier function of the skin (12).
The essential role of LA in barrier function was determined in several animal experiments similar to those conducted by Burr and Burr (1, 2). EFA deficiency (EFAD) was induced by feeding animals a hydrogenated coconut oil diet (which completely lacks EFAs), and the ability of specific fatty acid species to rescue the cutaneous and biochemical symptoms of EFAD was assessed. Supplementation with safflower or primrose oil corrected the deficiency symptoms, while supplementation with menhaden fish oil had no effect (Table 2) (13, 14). Purified LA preparations could also rescue barrier function in EFAD rats (12) and mice (15), whereas omega-3-rich preparations had no effect. These studies confirm the specific role of omega-6 PUFAs, and LA in particular, on skin barrier function.
Arachidonic acid (AA) is the second most abundant PUFA in the epidermis, accounting for approximately 9% of total epidermal fatty acids (10). It is a structural component of phosphatidylinositol and phosphatidylserine, phospholipids found in the membranes of epidermal keratinocytes. AA can be released from phospholipids by the enzyme phospholipase A2 (PLA2) and serves as the major source of epidermal eicosanoids, potent mediators of the inflammatory response (7, 13).
Omega-3 EFAs comprise less than 2% of total epidermal fatty acids (12, 16). Although they do not appreciably accumulate in the skin, n-3 fatty acids serve an important immunomodulatory role (17). Moreover, dietary supplementation can enrich long chain n-3 fatty acids in the epidermis, significantly altering the fatty acid composition and eicosanoid content of the skin (18, 19).
The main function of the dermis is to provide physical and nutritional support to the epidermis (5). The role of EFAs in the dermis appears to be related to their production of signaling molecules that mediate the inflammatory response. Damage to dermal collagen governs skin aging, and n-3 EFAs may attenuate UV-induced photoaging via signal transduction cascades that minimize collagen damage (see Photoaging).
Additionally, there is evidence that fatty acid metabolites produced in the dermis can act on cells in the epidermis (20, 21). Purified extracts and fibroblasts from normal human skin have been used to study AA metabolism in the dermis. From these studies, the anti-inflammatory eicosanoid 15-HETE was identified as the major AA metabolite in the dermis and was shown to inhibit the formation of the pro-inflammatory eicosanoid 12-HETE in the epidermis (20). Interestingly, interaction between the dermis and epidermis appears to be central to psoriasis, an inflammatory skin condition characterized by epidermal hyperproliferation and plaque formation (21). This article focuses on healthy skin, however, and does not elaborate on the relationship between EFAs and various skin disorders.
Skin is a metabolically active organ. Saturated fatty acids, monounsaturated fatty acids (MUFAs), cholesterol, and ceramides can be synthesized and modified in the skin; however, EFAs must be obtained from exogenous sources. Furthermore, unlike the liver, the skin lacks the enzymatic machinery required for conversion of LA and ALA to their long-chain metabolites. Specifically, there is a deficiency in delta-6 and delta-5 desaturase activity, enzymes that add double bonds to fatty acid chains, thereby converting LA to γ-linolenic acid (GLA) and arachidonic acid (AA), and ALA to eicosapentaenoic acid (EPA) (Figure 1) (9, 10). Because of the inability of skin to produce these long-chain metabolites, GLA, AA, EPA, and DHA are also considered essential nutrients for the skin (9).
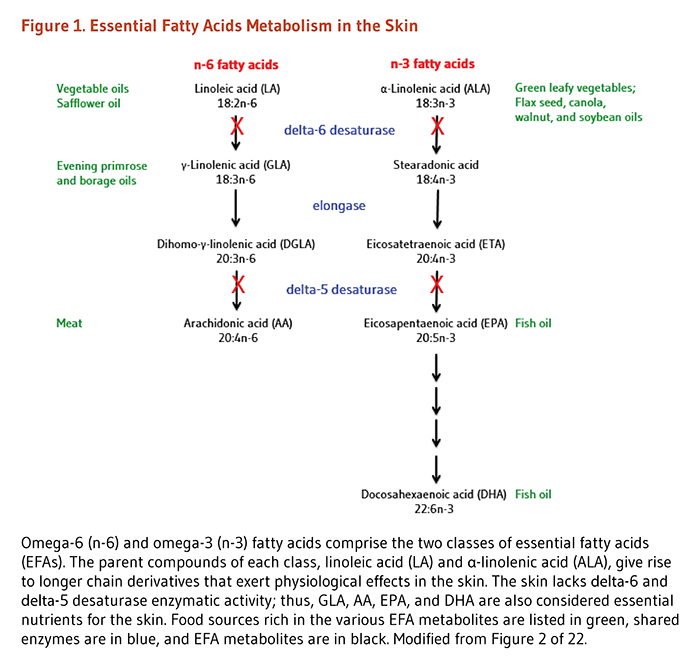
Although there is no detectable desaturase activity, elongase activity is retained in the epidermis (9, 10). Thus, dihomo-γ-linolenic acid (DGLA) can be synthesized from GLA in the epidermis when GLA is supplied exogenously. DGLA metabolites are thought to possess anti-inflammatory properties, thus several studies have investigated the effect of topical and dietary supplementation with GLA-rich oils on inflammatory skin conditions (5, 16, 22).
Eicosanoids are a large class of signaling molecules that includes prostaglandins (PGs), thromboxanes, leukotrienes, mono-and poly-hydroxy fatty acids, and lipoxins. These compounds are produced from n-6 and n-3 PUFAs by the action of enzymes known as cyclooxygenases (COX) and lipoxygenases (LOX) (Figure 2) (23).
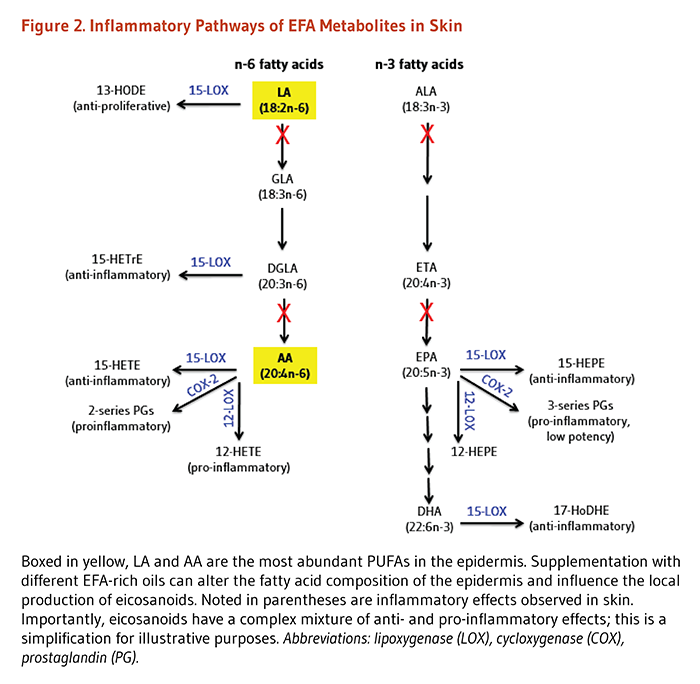
The skin expresses two cyclooxygenase isoforms: constitutive COX-1 and inducible COX-2. COX-2 is induced in response to reactive oxygen species (ROS) and ultraviolet radiation (UVR), resulting in the increased production of prostaglandins from AA and EPA substrates (24). Specifically, AA is converted to PGE2, a major contributor to UV-induced inflammation and immunosuppression. EPA is converted to PGE3, a less potent inflammatory eicosanoid. Increasing the availability of EPA, either through diet or topical application, shifts the PUFA and eicosanoid content of the skin to an n-3 profile, thereby attenuating the negative effects of UV exposure (see Photoprotection).
Mammalian skin expresses 5-, 12-, and 15-lipoxygenase (LOX) enzyme isoforms (25). LOX enzymes produce eicosanoids known as hydroxy fatty acids from omega-3 and omega-6 PUFAs (see Figure 2 above). 5- and 12-LOX produce monohydroxy fatty acids with potent chemoattractant and proinflammatory effects; 15-LOX products, on the other hand, display antiproliferative and anti-inflammatory effects in skin (25).
Experiments using human keratinocyte cell cultures and isolated skin extracts demonstrate that UV exposure reduces 12-LOX expression but increases 15-LOX expression (26). Furthermore, 15-LOX metabolites inhibit 12-LOX expression and the formation of its proinflammatory product, 12-HETE (20, 26). Notably, COX-2 is also induced by UVR, and there is an orchestrated expression pattern of COX- and LOX-derived eicosanoids that mediate the response to UVR (see Photoprotection) (27).
In addition to UV exposure, dietary interventions can influence the eicosanoid content of skin. Feeding corn oil or safflower oil (both rich in LA) to normal and EFA-deficient guinea pigs results in increased epidermal 13-HODE content (16) and the suppression of epidermal hyperproliferation characteristic of EFAD (28). EPA and DHA can also be converted into monohydroxy fatty acids by 15-LOX, forming 15-HEPE and 17-HoDHE, respectively (16). DGLA gives rise to 15-HETrE, which exerts the most potent in vitro anti-inflammatory effect among the monohydroxy fatty acids (22). Feeding studies in guinea pigs reveal that fish or borage oil supplementation can significantly alter both the fatty acid composition and levels of corresponding hydroxy fatty acid derivatives in the epidermis (29, 30). For this reason, supplementation with fish oil and GLA-rich oils has been investigated for treatment of inflammatory skin disorders like psoriasis, eczema, and atopic dermatitis.
In summary, there is a complex interaction between LOX- and COX-generated metabolites in the skin. UV exposure can influence LOX and COX enzyme activity, thus altering the types and ratios of eicosanoids produced from PUFA precursors. Dietary supplementation and topical application of certain PUFAs can enrich for a particular starting substrate, thus influencing the eicosanoids produced by LOX and COX both at baseline and in response to UV exposure.
Essential fatty acid deficiency (EFAD) significantly affects skin function and appearance. EFAD is characterized by hyperproliferation of the epidermis, dermatitis, and increased transepidermal water loss (TEWL). TEWL reflects the integrity of the barrier function of the skin and is directly related to the EFA composition of structural lipids in the stratum corneum.
In humans, dermatitis may not be present for weeks to months, while the biochemical signs of EFAD manifest within days to weeks (31). Biochemically, EFAD is characterized by the presence of mead acid (20:3n-9) in plasma phospholipids. During EFAD, mead acid is produced from the disproportionate abundance of omega-9 fatty acids in the absence of omega-6 and omega-3 fatty acids. Because mead acid is not produced in EFA-replete individuals, its presence in plasma and structural lipids in the skin is diagnostic of EFAD (see the article on Essential Fatty Acids).
The fatty acid composition of the skin can be significantly modified by the diet (13, 18, 29, 30, 32). Fats are absorbed across the intestine inside lipoprotein particles called chylomicrons and processed by the liver for delivery to peripheral tissues like the skin. Dietary EFAs can be delivered to the epidermis through cellular uptake by way of lipoprotein receptors and fatty acid transporters in epidermal keratinocytes (8, 17). Labeling studies in guinea pigs have shown that ingested ALA accumulates in skin and fur, in addition to muscle, bone, and adipose tissue (33, 34). Presumably dietary ALA accumulates in sebaceous glands before being delivered as free fatty acids to the fur and surface of the skin (34). As discussed more extensively in the sections below, oils rich in different fatty acid species have been used extensively in feeding studies in both animals and humans to evaluate the effect of EFAs on skin health (see Functions in Healthy Skin).
Topical application is also a successful route of EFA delivery to the skin. Symptoms of EFA deficiency (EFAD) in both animals (12, 15) and humans (4, 35) can be reversed by either topical application or ingestion of oils rich in LA.
Prottey et al. compared the efficacy of topically applied olive oil and sunflower seed oil to correct the cutaneous symptoms of EFAD in humans (4, 35). Sunflower seed oil (250 mg) increased the LA content of the epidermis, normalized TEWL, and reduced skin scaliness after two weeks of daily application to the forearm (4). None of these skin parameters were altered in the control subjects given topical sunflower seed oil in the absence of EFAD. The biochemical abnormalities of EFAD were also corrected by topical application of sunflower seed oil (35), indicating that cutaneously delivered EFAs eventually travel to the systemic circulation. Studies in EFAD animal models corroborate the observations in EFAD patients. After 15 days of applying safflower oil (approximately 1.5% of total caloric intake) to a small intrascapular area on EFAD rats, the LA and arachidonic acid (AA) content of red blood cell membranes and plasma phospholipids increased, while the mead acid content (a biochemical marker of EFAD) decreased (36).
Topical application of oil is an effective means of delivering EFAs to the skin and, eventually, to the rest of body. Because a significant portion of ingested EFAs may be oxidized by the liver (up to 60% of ALA and 20% of LA (37)) before reaching peripheral tissues, topical application may be a more efficient route of delivery for skin effects, especially during deficiency (35). Topical application of LA-rich oils has high clinical relevance in the treatment of EFAD in preterm infants, patients receiving total parenteral nutrition, situations of fat malabsorption, and at-risk individuals in the developing world. Importantly, not all oils are equally beneficial to skin barrier function in EFAD states. Darmstadt et al. (38) tested a variety of oils in a mouse model of EFAD. Sunflower seed oil enhanced skin barrier recovery, while mustard seed, olive, and soybean oils delayed skin barrier recovery and, in the case of mustard seed oil, damaged keratinocyte organelles and disrupted the architecture of the stratum corneum (38). Moreover, in normal guinea pigs, topical application of purified omega-3 fatty acids (0.5% EPA or 0.5% DHA) induced epidermal hyperproliferation after five days of daily application (37). The hyperproliferation is accompanied by a decline in 13-HODE, the major epidermal metabolite derived from LA in the epidermis (39).
Sunburn, also referred to as erythema, is caused by excess exposure to ultraviolet radiation (UVR). Even at levels that may not cause sunburn, UVR causes cellular damage that induces inflammation and suppresses the immune system in the skin (40, 41). Because both omega-6 and omega-3 EFAs are converted into compounds that participate in inflammatory and immune reactions, their levels in skin can influence the cellular response to UVR.
Topically applied sunscreens protect our skin from the damaging effects of UVR, but their influence is local and temporary, application may be incomplete, and the vast majority of UVR exposure occurs during non-vacation time, when many individuals forego sunscreen (40, 42, 43). There are a number of endogenous defense mechanisms in place to protect the skin from UVR, including melanin production, antioxidant defenses, and enzymatic repair pathways (see the article on Micronutrients and Skin Health). Evidence shows that dietary omega-3 PUFA supplementation provides an added layer of systemic photoprotection from the damaging effects of UVR (40, 41).
Photoprotection is assessed by measuring the Minimal Erythemal Dose (MED), the lowest dose of radiation that will produce a detectable erythema 24 hours after UVR exposure. In other words, the higher the MED, the more resistant the skin is to sunburn. Results of several placebo-controlled trials indicate that oral supplementation with fish oil increases the MED in healthy individuals. In one trial, 20 healthy men and women (median age, 36 years) ingested either placebo or fish oil capsules (2.8 g DHA and 1.2 g EPA per day) for four weeks (44). Compared to placebo, there was a significant reduction in UVB-induced erythema in subjects consuming supplemental fish oil. In a second controlled trial, Rhodes et al. (18) gave ten healthy, Caucasian volunteers (median age, 42 years) 5 g of fish oil twice daily for six months. Fish oil supplementation increased the omega-3 content of the skin and progressively increased the MED throughout the supplementation period. Once fish oil supplementation was terminated, the MED value returned to baseline. A third randomized-controlled trial investigated the effect of purified EPA on UV-response. Forty-two healthy Caucasian men and women (median age, 44 years) ingested 4 g/day of purified EPA or oleic acid for three months (19). EPA supplementation led to an 8-fold increase in the EPA content of the skin, increased the MED, and reduced UVR-induced expression of p53 (a marker of DNA damage) compared to those consuming oleic acid.
Topically applied omega-3 fatty acids may also attenuate the UV-response. In a small human trial, ten healthy men and women (aged 25-35 years) received sardine oil extract (200 mg) applied topically to six sites on the ventral surface of their forearms, followed by UVB exposure at two times their MED (45). Topical application of sardine oil extract (rich in EPA and DHA) reduced UVB-induced erythema compared to control sites on each subjects forearm. Consistent with this outcome, topical application of the n-3 fatty acid eicosatrienoic acid (20:3n-3) protected against UV-induced skin damage in hairless mice (46). Another animal study, however, reported that dietary, but not topical, ALA suppressed UVB-induced erythema and accumulation of the inflammatory eicosanoid, prostaglandin E2 (PGE2) in hairless mice (47).
Omega-3 EFAs protect against the damaging effects of sunlight by modulating the UVR-induced inflammatory response in the skin. UVB exposure activates phospholipase A2 (PLA2), an enzyme that cleaves fatty acids from membrane-bound phospholipids (24). As mentioned above, arachidonic acid (AA) is the second most abundant PUFA in the epidermis and the major source of epidermal eicosanoids. UVB thus liberates AA from epidermal cell membranes, making it available for conversion to pro-inflammatory prostaglandins in the skin (27).
Dietary supplementation with fish oil influences the fatty acid composition of the epidermis, enriching for EPA in membrane phospholipids (18, 19). As a result, UV-liberated EPA can compete with AA as substrate for COX and LOX action, thereby decreasing the production of pro-inflammatory AA-derived prostaglandins (23, 48) (see Figure 2 above). In support of this concept, in a double-blind randomized placebo-controlled trial with 48 healthy volunteers, fish oil supplementation protected against sunburn (i.e., increased the MED) and prevented the induction of PGE2 following UVB exposure (49). Thus, the overall effect of n-3 supplementation is to suppress the inflammatory response following UVR exposure, potentially through competitive inhibition with n-6 fatty acids (40, 41, 50).
Among the many deleterious effects of UVR on skin, UVB also suppresses the immune system by impairing T-cell activation and lowering the numbers Langerhans cells—epidermal immune cells involved in antigen presentation and contact hypersensitivity response (51). PGE2 production from AA (via COX-2) contributes to both inflammation and immunosuppression following UVB exposure.
There is evidence that photoprotection by n-3 PUFAs relies on a balance between inflammatory, immune, and antioxidant systems in the skin. In mouse epidermis, topical EPA (10 nmol/cm2, 30 min) protected against UVB-induced immunosuppression, but also increased lipid peroxidation and decreased vitamin C levels compared to oleic acid treated control mice (52). Similarly, dietary EPA supplementation (20% of total fatty acids consumed daily for ten days) protected skin from UVB-induced immunosuppression but increased lipid peroxidation and reduced vitamin C and glutathione levels in mouse epidermis (53).
EPA supplementation enriches for n-3 PUFAs and lower potency 3-series prostaglandins in the skin, thus attenuating inflammation and immunosuppression following UVB exposure. However, long-chain omega-3 PUFAs are highly susceptible to oxidation due to their chemical structure (i.e., the presence of multiple double bonds) and may therefore put an extra demand on the antioxidant systems in the skin (see the article on Vitamin C and Skin Health). Maintenance of antioxidant status of the skin thus appears to be an important prerequisite for the photoprotective effect of EPA.
Skin aging is classified into two types: extrinsic photoaging is due to external influences, mainly UV exposure and smoking; intrinsic chronological skin aging results from time and genetics. Photoaging is characterized by morphological (shape) and histological (tissue) changes to the skin, including deep wrinkling, loss of elasticity, altered pigmentation, and collagen destruction (54).
Cross-sectional studies have reported that higher dietary intakes of EFAs are associated with more youthful skin appearance and photoprotection. Purba et al. (55) investigated the association between skin wrinkling in a sun-exposed site (back of hand) and types of food ingested in 453 older women (≥70 years). Higher intakes of vegetables, olive oil, MUFAs, and legumes and lower intakes of milk/milk products, butter, margarine, and sugar products were associated with less skin wrinkling in a sun-exposed site. Combining intake data from The National Health and Nutritional Examination Survey (NHANES) I with a dermatological visit, Cosgrove et al. (56) found that higher dietary intakes of LA were associated with a lower incidence of dry skin and skin thinning in healthy, middle-aged women (40-74 years old).
Destruction of collagen, the major structural component of the dermis, is thought to underlie skin aging (57). In addition to initiating an inflammatory response, UVR causes physical damage to collagen through its induction of matrix metalloproteases (MMPs). MMPs are enzymes secreted by epidermal keratinocytes and dermal fibroblasts in response to various stimuli, including UVR, oxidative stress, and inflammatory cytokines. UVR induces three MMPs: MMP-1 (collagenase), MMP-3, (stomelysin), and MMP-9 (gelatinase) that cleave and degrade skin collagen (58).
In cell culture experiments, pretreatment with EPA (5 micromoles, 24 hours) inhibits UV-induced MMP-1 expression in human dermal fibroblasts, suggesting that EPA may reduce collagen damage associated with photoaging by preventing MMP-1 induction (59). To assess the effect of EPA on skin aging in humans, a small study was performed in seven young (20-30 years of age) and four elderly (≥75 years old) healthy male subjects in a sun-protected site (60). Compared to a vehicle-treated site on the same subject, topical application of 2% EPA attenuated UV-induced MMP-1 and -9 expression and epidermal thickening, and increased collagen and elastic fiber expression in young skin. In older men, two weeks of EPA application increased dermal expression of procollagen, tropoelastin, and fibrillin-1—proteins that contribute to collagen synthesis and repair. These results suggest that EPA may exert a protective effect on both extrinsic and intrinsic skin aging.
Among its many deleterious effects on skin, UVR also induces hyperpigmentation. To assess the effect of topical EFA treatment on hyperpigmentation, Ando et al. (61) established UVB-induced hyperpigmentation in guinea pigs (UVB exposure three times/week for two weeks) and then applied oleic acid, LA, or ALA (0.5%, five times/week for three weeks) to the hyperpigmented areas. There was a decline in UV-induced hyperpigmentation after three weeks of treatment with all fatty acid formulations, with the strongest lightening effect observed with LA. The lightening effect was not due to the destruction of melanocytes or increased turnover of the stratum corneum.
A few intervention trials have investigated the effect of EFA-rich oils on various parameters related to dry and sensitive skin in healthy subjects. In one placebo-controlled trial (62), 45 women (aged 18 to 65 years old) with dry and sensitive skin were assigned to one of three treatment groups: placebo, flaxseed oil (rich in ALA), or borage oil (rich in GLA) ingested as four capsules per day (2.2 g total) for 12 weeks. Compared to placebo, both oils significantly improved all skin properties measured. Specifically, there was attenuated inflammatory response to a chemical skin irritant, decreased TEWL, and reduced skin roughness and scaling. Another placebo-controlled study (63) investigated the effect of evening primrose oil (rich in GLA) on skin parameters in 40 healthy adult men and women (aged 32 to 56 years old). After 12 weeks, subjects consuming 1.5 g of evening primrose oil per day had significant improvements in skin moisture, TEWL, elasticity, firmness, and roughness compared to placebo.
It is difficult to attribute a beneficial effect on skin sensitivity to a specific EFA as the oils used in these trials contain a mixture of fatty acid species. Flaxseed oil is a rich source of ALA but also contains LA and oleic acid. Borage and evening primrose oils are rich in GLA but also contain LA and oleic acid (see Table 2 above) (62, 64).
Given their roles in structural integrity and modulation of the inflammatory response in the skin, it seems likely that EFAs might influence the orchestrated response to wounding (see the article on Micronutrients and Skin Health). Wound healing is roughly divided into three overlapping phases: inflammation, tissue formation, and tissue remodeling (65). Early on, inflammation is necessary to clear foreign particles and initiate new tissue formation. Chronic inflammation, on the other hand, may be detrimental and delay the healing process.
Two placebo-controlled trials have investigated the effect of fish oil supplementation on epidermal wound healing in humans (66, 67). In the first trial, 30 healthy volunteers (18-45 years old) ingested placebo or fish oil (1.6 g EPA, 1.1 g DHA) daily for 28 days (66). In the second trial, 18 healthy volunteers (18-45 years old) ingested placebo or fish oil (1.6 g EPA, 1.2 g DHA) daily for 28 days; both treatment groups also ingested 81 mg aspirin (67). A similar study design was used in both trials in which blisters were created on subject’s forearms, and blister fluid content and wound area were monitored at baseline and up to approximately 15 days post-wounding. In both trials, supplementation with fish oil shifted the fatty acid and eicosanoid content at the site of wounding to an n-3 profile and improved the healing process.
Animal studies investigating EFA supplementation on wound healing have reported mixed results. Cardoso et al. (68) investigated the effect of topical application of purified n-3, n-6, and n-9 fatty acids (30 micromoles/day for 20 days) on surgically induced wound closure in mice. Topical application of oleic acid accelerated while ALA delayed wound closure. In another study, feeding rats n-3-rich fish oil diets (17% menhaden oil) resulted in weakened mechanical properties at the site of wound repair compared to rats fed n-6-rich corn oil diets (69). Approaching the question from a different angle, Porras-Reyes et al. (70) induced EFA deficiency (EFAD) in rats before surgical wounding. The healing response was then compared between normal, EFAD, and recovered EFAD rats for up to 21 days post-wounding. Replete and EFAD rats exhibited the same course of histological and immunological changes in response to wounding, suggesting that EFA status does not influence the wound-healing process.
Omega-6 (n-6) and omega-3 (n-3) essential fatty acids (EFAs) are crucial to skin function and appearance. Both dietary and topical supplementation with EFAs can have profound effects on the fatty acid composition and eicosanoid milieu of the skin. As a result, addition of various EFA-rich oils (see Table 2 above) can modulate the inflammatory response in both dermal and epidermal layers of the skin. Supplementation with n-3 fatty acids in particular exerts protection from photodamage and photoaging. There is some evidence that n-3 supplementation adversely affects wound healing, but further research is necessary to address this question. N-6 EFAs are required for skin barrier function and structural integrity. Supplementation with n-6 fatty acids alleviates symptoms associated with skin sensitivity and inflammatory skin disorders. The mechanism by which EFAs influence skin reactions is likely through changes in the ratio of pro- and anti-inflammatory eicosanoids derived from EFA precursors. N-6 and n-3 fatty acids compete for the same enzymes; thus supplementation with specific EFAs can alter the corresponding metabolites, significantly influencing skin function and appearance.
Written in February 2012 by:
Giana Angelo, Ph.D.
Linus Pauling Institute
Oregon State University
Reviewed in February 2012 by:
Suzanne Pilkington, Ph.D.
Dermatological Sciences, Inflammation Research Group,
School of Translational Medicine
The University of Manchester
This article was underwritten, in part, by a grant from Neutrogena Corporation, Los Angeles, California.
Copyright 2012-2024 Linus Pauling Institute
1. Burr GO, Burr MM. A new deficiency disease produced by the rigid exclusion of fat from the diet. J Biol Chem. 1929;82:345-367.
2. Burr GO, Burr MM. On the nature and role of the fatty acids essential in nutrition. J Biol Chem. 1930;86:587-621.
3. Hansen AE, Haggard ME, Boelsche AN, Adam DJ, Wiese HF. Essential fatty acids in infant nutrition. III. Clinical manifestations of linoleic acid deficiency. J Nutr. 1958;66:565-576. (PubMed)
4. Prottey C, Hartop PJ, Press M. Correction of the cutaneous manifestations of essential fatty acid deficiency in man by application of sunflower-seed oil to the skin. J Invest Dermatol. 1975;64:228-234. (PubMed)
5. Ziboh VA, Chapkin RS. Metabolism and function of skin lipids. Prog Lipid Res. 1988;27:81-105. (PubMed)
6. Gray GM, Yardley HJ. Different populations of pig epidermal cells: isolation and lipid composition. J Lipid Res. 1975;16:441-447. (PubMed)
7. Wertz PW. Epidermal lipids. Semin Dermatol. 1992;11:106-113. (PubMed)
8. Feingold KR. The outer frontier: the importance of lipid metabolism in the skin. J Lipid Res. 2009;50 Suppl:S417-422. (PubMed)
9. Chapkin RS, Ziboh VA. Inability of skin enzyme preparations to biosynthesize arachidonic acid from linoleic acid. Biochem Biophys Res Commun. 1984;124:784-792. (PubMed)
10. Chapkin RS, Ziboh VA, Marcelo CL, Voorhees JJ. Metabolism of essential fatty acids by human epidermal enzyme preparations: evidence of chain elongation. J Lipid Res. 1986;27:945-954. (PubMed)
11. Gray GM, Yardley HJ. Lipid compositions of cells isolated from pig, human, and rat epidermis. J Lipid Res. 1975;16:434-440. (PubMed)
12. Hansen HS, Jensen B. Essential function of linoleic acid esterified in acylglucosylceramide and acylceramide in maintaining the epidermal water permeability barrier. Evidence from feeding studies with oleate, linoleate, arachidonate, columbinate and alpha-linolenate. Biochim Biophys Acta. 1985;834:357-363. (PubMed)
13. Chapkin RS, Ziboh VA, McCullough JL. Dietary influences of evening primrose and fish oil on the skin of essential fatty acid-deficient guinea pigs. J Nutr. 1987;117:1360-1370. (PubMed)
14. Ziboh VA, Chapkin RS. Biologic significance of polyunsaturated fatty acids in the skin. Arch Dermatol. 1987;123:1686a-1690. (PubMed)
15. Elias PM, Brown BE, Ziboh VA. The permeability barrier in essential fatty acid deficiency: evidence for a direct role for linoleic acid in barrier function. J Invest Dermatol. 1980;74:230-233. (PubMed)
16. Ziboh VA, Miller CC, Cho Y. Metabolism of polyunsaturated fatty acids by skin epidermal enzymes: generation of antiinflammatory and antiproliferative metabolites. Am J Clin Nutr. 2000;71:361S-366S. (PubMed)
17. McCusker MM, Grant-Kels JM. Healing fats of the skin: the structural and immunologic roles of the omega-6 and omega-3 fatty acids. Clin Dermatol. 2010;28:440-451. (PubMed)
18. Rhodes LE, O'Farrell S, Jackson MJ, Friedmann PS. Dietary fish-oil supplementation in humans reduces UVB-erythemal sensitivity but increases epidermal lipid peroxidation. J Invest Dermatol. 1994;103:151-154. (PubMed)
19. Rhodes LE, Shahbakhti H, Azurdia RM, et al. Effect of eicosapentaenoic acid, an omega-3 polyunsaturated fatty acid, on UVR-related cancer risk in humans. An assessment of early genotoxic markers. Carcinogenesis. 2003;24:919-925. (PubMed)
20. Kragballe K, Pinnamaneni G, Desjarlais L, Duell EA, Voorhees JJ. Dermis-derived 15-hydroxy-eicosatetraenoic acid inhibits epidermal 12-lipoxygenase activity. J Invest Dermatol. 1986;87:494-498. (PubMed)
21. Saiag P, Coulomb B, Lebreton C, Bell E, Dubertret L. Psoriatic fibroblasts induce hyperproliferation of normal keratinocytes in a skin equivalent model in vitro. Science. 1985;230:669-672. (PubMed)
22. Ziboh VA, Cho Y, Mani I, Xi S. Biological significance of essential fatty acids/prostanoids/lipoxygenase-derived monohydroxy fatty acids in the skin. Arch Pharm Res. 2002;25:747-758. (PubMed)
23. Lands WE. Biochemistry and physiology of n-3 fatty acids. Faseb J. 1992;6:2530-2536. (PubMed)
24. Hruza LL, Pentland AP. Mechanisms of UV-induced inflammation. J Invest Dermatol. 1993;100:35S-41S. (PubMed)
25. Ziboh VA. Prostaglandins, leukotrienes, and hydroxy fatty acids in epidermis. Semin Dermatol. 1992;11:114-120. (PubMed)
26. Yoo H, Jeon B, Jeon MS, Lee H, Kim TY. Reciprocal regulation of 12- and 15-lipoxygenases by UV-irradiation in human keratinocytes. FEBS Lett. 2008;582:3249-3253. (PubMed)
27. Rhodes LE, Gledhill K, Masoodi M, et al. The sunburn response in human skin is characterized by sequential eicosanoid profiles that may mediate its early and late phases. Faseb J. 2009;23:3947-3956. (PubMed)
28. Cho Y, Ziboh VA. Nutritional modulation of guinea pig skin hyperproliferation by essential fatty acid deficiency is associated with selective down regulation of protein kinase C-beta. J Nutr. 1995;125:2741-2750. (PubMed)
29. Miller CC, Tang W, Ziboh VA, Fletcher MP. Dietary supplementation with ethyl ester concentrates of fish oil (n-3) and borage oil (n-6) polyunsaturated fatty acids induces epidermal generation of local putative anti-inflammatory metabolites. J Invest Dermatol. 1991;96:98-103. (PubMed)
30. Miller CC, Ziboh VA, Wong T, Fletcher MP. Dietary supplementation with oils rich in (n-3) and (n-6) fatty acids influences in vivo levels of epidermal lipoxygenase products in guinea pigs. J Nutr. 1990;120:36-44. (PubMed)
31. Jeppesen PB, Hoy CE, Mortensen PB. Essential fatty acid deficiency in patients receiving home parenteral nutrition. Am J Clin Nutr. 1998;68:126-133. (PubMed)
32. Oikawa D, Nakanishi T, Nakamura Y, et al. Dietary CLA and DHA modify skin properties in mice. Lipids. 2003;38:609-614. (PubMed)
33. Fu Z, Sinclair AJ. Increased alpha-linolenic acid intake increases tissue alpha-linolenic acid content and apparent oxidation with little effect on tissue docosahexaenoic acid in the guinea pig. Lipids. 2000;35(4):395-400. (PubMed)
34. Fu Z, Sinclair AJ. Novel pathway of metabolism of alpha-linolenic acid in the guinea pig. Pediatric research. 2000;47(3):414-417. (PubMed)
35. Press M, Hartop PJ, Prottey C. Correction of essential fatty-acid deficiency in man by the cutaneous application of sunflower-seed oil. Lancet. 1974;1:597-598. (PubMed)
36. Bohles H, Bieber MA, Heird WC. Reversal of experimental essential fatty acid deficiency by cutaneous administration of safflower oil. Am J Clin Nutr. 1976;29:398-401. (PubMed)
37. Sinclair AJ, Attar-Bashi NM, Li D. What is the role of alpha-linolenic acid for mammals? Lipids. 2002;37:1113-1123. (PubMed)
38. Darmstadt GL, Mao-Qiang M, Chi E, et al. Impact of topical oils on the skin barrier: possible implications for neonatal health in developing countries. Acta Paediatr. 2002;91:546-554. (PubMed)
39. Miller CC, Ziboh VA. Induction of epidermal hyperproliferation by topical n-3 polyunsaturated fatty acids on guinea pig skin linked to decreased levels of 13-hydroxyoctadecadienoic acid (13-hode). J Invest Dermatol. 1990;94:353-358. (PubMed)
40. Pilkington SM, Watson RE, Nicolaou A, Rhodes LE. Omega-3 polyunsaturated fatty acids: photoprotective macronutrients. Exp Dermatol. 2011;20:537-543. (PubMed)
41. Sies H, Stahl W. Nutritional protection against skin damage from sunlight. Annu Rev Nutr. 2004;24:173-200. (PubMed)
42. Bech-Thomsen N, Wulf HC. Sunbathers' application of sunscreen is probably inadequate to obtain the sun protection factor assigned to the preparation. Photodermatol Photoimmunol Photomed. 1992;9:242-244. (PubMed)
43. Godar DE, Wengraitis SP, Shreffler J, Sliney DH. UV doses of Americans. Photochem Photobiol. 2001;73:621-629. (PubMed)
44. Orengo IF, Black HS, Wolf JE, Jr. Influence of fish oil supplementation on the minimal erythema dose in humans. Arch Dermatol Res. 1992;284:219-221. (PubMed)
45. Puglia C, Tropea S, Rizza L, Santagati NA, Bonina F. In vitro percutaneous absorption studies and in vivo evaluation of anti-inflammatory activity of essential fatty acids (EFA) from fish oil extracts. Int J Pharm. 2005;299:41-48. (PubMed)
46. Jin XJ, Kim EJ, Oh IK, et al. Prevention of UV-induced skin damages by 11,14,17-eicosatrienoic acid in hairless mice in vivo. J Korean Med Sci. 2010;25:930-937. (PubMed)
47. Takemura N, Takahashi K, Tanaka H, et al. Dietary, but not topical, alpha-linolenic acid suppresses UVB-induced skin injury in hairless mice when compared with linoleic acids. Photochem Photobiol. 2002;76:657-663. (PubMed)
48. James MJ, Gibson RA, Cleland LG. Dietary polyunsaturated fatty acids and inflammatory mediator production. Am J Clin Nutr. 2000;71:343S-348S. (PubMed)
49. Shahbakhti H, Watson RE, Azurdia RM, et al. Influence of eicosapentaenoic acid, an omega-3 fatty acid, on ultraviolet-B generation of prostaglandin-E2 and proinflammatory cytokines interleukin-1 beta, tumor necrosis factor-alpha, interleukin-6 and interleukin-8 in human skin in vivo. Photochem Photobiol. 2004;80:231-235. (PubMed)
50. Boelsma E, Hendriks HF, Roza L. Nutritional skin care: health effects of micronutrients and fatty acids. Am J Clin Nutr. 2001;73:853-864. (PubMed)
51. Aubin F. Mechanisms involved in ultraviolet light-induced immunosuppression. Eur J Dermatol. 2003;13:515-523. (PubMed)
52. Moison RM, Steenvoorden DP, Beijersbergen van Henegouwen GM. Topically applied eicosapentaenoic acid protects against local immunosuppression induced by UVB irradiation, cis-urocanic acid and thymidine dinucleotides. Photochem Photobiol. 2001;73:64-70. (PubMed)
53. Moison RM, Beijersbergen Van Henegouwen GM. Dietary eicosapentaenoic acid prevents systemic immunosuppression in mice induced by UVB radiation. Radiat Res. 2001;156:36-44. (PubMed)
54. Gilchrest BA. Skin aging and photoaging: an overview. J Am Acad Dermatol. 1989;21:610-613. (PubMed)
55. Purba MB, Kouris-Blazos A, Wattanapenpaiboon N, et al. Skin wrinkling: can food make a difference? J Am Coll Nutr. 2001;20:71-80. (PubMed)
56. Cosgrove MC, Franco OH, Granger SP, Murray PG, Mayes AE. Dietary nutrient intakes and skin-aging appearance among middle-aged American women. Am J Clin Nutr. 2007;86:1225-1231. (PubMed)
57. Braverman IM, Fonferko E. Studies in cutaneous aging: I. The elastic fiber network. J Invest Dermatol. 1982;78:434-443. (PubMed)
58. Fisher GJ, Kang S, Varani J, et al. Mechanisms of photoaging and chronological skin aging. Arch Dermatol. 2002;138:1462-1470. (PubMed)
59. Kim HH, Shin CM, Park CH, et al. Eicosapentaenoic acid inhibits UV-induced MMP-1 expression in human dermal fibroblasts. J Lipid Res. 2005;46:1712-1720. (PubMed)
60. Kim HH, Cho S, Lee S, et al. Photoprotective and anti-skin-aging effects of eicosapentaenoic acid in human skin in vivo. J Lipid Res. 2006;47:921-930. (PubMed)
61. Ando H, Ryu A, Hashimoto A, Oka M, Ichihashi M. Linoleic acid and alpha-linolenic acid lightens ultraviolet-induced hyperpigmentation of the skin. Arch Dermatol Res. 1998;290:375-381. (PubMed)
62. De Spirt S, Stahl W, Tronnier H, et al. Intervention with flaxseed and borage oil supplements modulates skin condition in women. Br J Nutr. 2009;101:440-445. (PubMed)
63. Muggli R. Systemic evening primrose oil improves the biophysical skin parameters of healthy adults. Int J Cosmet Sci. 2005;27:243-249. (PubMed)
64. Neukam K, De Spirt S, Stahl W, et al. Supplementation of flaxseed oil diminishes skin sensitivity and improves skin barrier function and condition. Skin Pharmacol Physiol. 2011;24:67-74. (PubMed)
65. Singer AJ, Clark RA. Cutaneous wound healing. N Engl J Med. 1999;341:738-746. (PubMed)
66. McDaniel JC, Belury M, Ahijevych K, Blakely W. Omega-3 fatty acids effect on wound healing. Wound Repair Regen 2008;16:337-345. (PubMed)
67. McDaniel JC, Massey K, Nicolaou A. Fish oil supplementation alters levels of lipid mediators of inflammation in microenvironment of acute human wounds. Wound Repair Regen. 2011;19:189-200. (PubMed)
68. Cardoso CR, Souza MA, Ferro EA, Favoreto S, Jr., Pena JD. Influence of topical administration of n-3 and n-6 essential and n-9 nonessential fatty acids on the healing of cutaneous wounds. Wound Repair Regen. 2004;12:235-243. (PubMed)
69. Albina JE, Gladden P, Walsh WR. Detrimental effects of an omega-3 fatty acid-enriched diet on wound healing. JPEN J Parenter Enteral Nutr. 1993;17:519-521. (PubMed)
70. Porras-Reyes BH, Schreiner GF, Lefkowith JB, Mustoe TA. Essential fatty acids are not required for wound healing. Prostaglandins Leukot Essent Fatty Acids. 1992;45:293-298. (PubMed)
Today is Dam Proud Day, the annual day of giving for Oregon State University.
You can help sustain the Micronutrient Information Center by making a gift of $5 or more today!