Contents
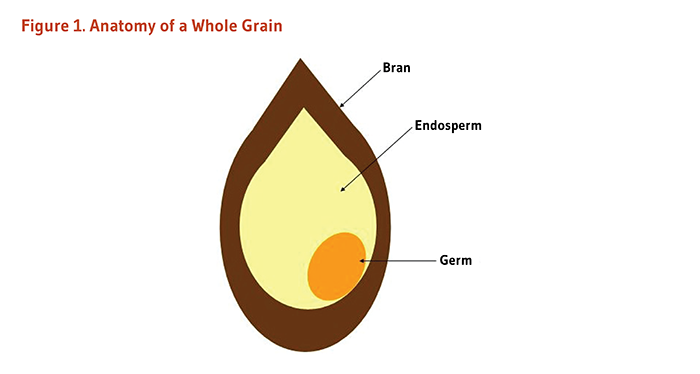
Grains are seeds of plants belonging to the Poaceae family (also called Gramineae or true grasses). Some examples of edible grains include wheat, rice, maize (corn), barley, oats, rye, triticale (wheat-rye hybrid), millet, bulgur, and sorghum (1). Although they are not members of the Poaceae family, whole-grain ingredients also include pseudo-grains like quinoa, amaranth, and buckwheat. A whole grain has an outer layer of bran, a carbohydrate-rich middle layer called the endosperm, and an inner germ layer (Figure 1). Whole-grain foods contain entire grain seeds either intact, cracked, crushed, or flaked, as long as the bran, endosperm, and germ are retained in the same proportions as they exist in the intact kernel (1). Whole grains are rich in potentially beneficial compounds, including vitamins, minerals, fiber, and phytochemicals, such as lignans and phytosterols (2). Most of these compounds are located in the bran or the germ of the grain, both of which are lost during the refining (milling) process, leaving only the starchy endosperm (1). Compared to diets high in refined grains, diets rich in whole grains are associated with reduced risks of several chronic diseases. The health benefits of whole grains are not entirely explained by the individual contributions of the nutrients and phytochemicals they contain. Whole grains represent a unique package of energy, micronutrients, and phytochemicals that work synergistically to promote health and prevent disease (3).
Because there is no globally accepted definition as to what constitutes a whole-grain food, it is difficult to compare studies that examined the effects of whole-grain consumption on markers of health and disease outcomes. The US Food and Drug Administration (FDA) approved health claims for whole grains (see Finding whole grain foods) to foods containing ≥51% of whole-grain ingredients by weight or ≥8 g of whole grains per one ounce (~30 g)-serving size (4). An international multidisciplinary expert group recently proposed to label "whole grain" a food with a whole-grain content of ≥8 g per ounce (5). Yet, to date, most epidemiological studies that examined the health impact of consuming whole-grain foods have included foods containing ≥25% of whole grains and added brans by weight (6).
A recent meta-analysis of eight large prospective cohort studies, including 385,868 participants, have found that high versus low intakes of total grains and whole grains were associated with a significant reduction in the risk of developing type 2 diabetes mellitus (7). On the other hand, no relationship was found between refined-grain intake and diabetes in a meta-analysis of six prospective studies of 258,078 subjects (7). Specifically, the consumption of three daily servings of whole-grain foods was associated with a 32% lower risk of diabetes (see below for Examples of one serving of whole grains). Further analyses showed a significantly lower risk of diabetes with high versus low consumption of whole grains as a single food (i.e., brown rice, wheat bran) or as an ingredient in food (i.e., whole-grain bread, whole-grain breakfast cereal) but not with refined grains like white rice and wheat germ (7). In addition, a pooled analysis of three large prospective cohorts — the Health Professionals Follow-up Study [HPFS] and the Nurses’ Health Studies [NHS I and II] — reported a 17% increased risk of type 2 diabetes in participants in the highest (≥5 servings/week) versus lowest (<1 serving/month) quintile of white rice intake, while brown rice consumption (≥2 servings/week versus <1 serving/month) was associated with an 11% reduction in risk (8). Interestingly, substituting 50 g/day (⅔ serving/day) of brown rice or other whole grains for the same amount of white rice could be associated with a predicted diabetes risk reduction of 16% or more (8).
Whole grains have been hypothesized to reduce the risk of type 2 diabetes mellitus by improving postprandial glycemia. Immediately after a meal, blood glucose and lipid concentrations are increased, and secretion of insulin by the pancreas stimulates glucose and lipid storage into tissues. Prolonged postprandial hyperglycemia and hyperlipidemia have been associated with oxidative stress, inflammation, insulin resistance, and endothelial dysfunction, all contributing to the development of chronic diseases like type 2 diabetes mellitus (9). The refining process that removes bran and germ facilitates the digestion of the carbohydrate-rich endosperm such that carbohydrates from refined grains were thought to elicit a higher and more rapid elevation in blood glucose, as well as a greater demand for insulin, than whole grains (10). However, compared with foods made from refined grains, whole-grain products do not necessarily have a lower glucose-raising potential, i.e., a lower glycemic index (GI) (11). The GI concept is based on the idea that foods containing carbohydrates that are easily digested, absorbed, and metabolized have a high GI (GI ≥70 on the glucose scale); in contrast, foods containing slowly digestible carbohydrates that elicit a reduced postprandial glucose response are considered to have a low GI (GI ≤55 on the glucose scale) (see also the article on Glycemic Index and Glycemic Load) (12). Bread, breakfast cereal, rice, and snack products have been attributed either a low or high GI, whether or not they include whole grains (11), suggesting that the type of food rather than its whole-grain content affects postprandial blood glucose concentrations.
In some observational studies, higher whole-grain intakes have been associated with decreased insulin resistance (13) and increased insulin sensitivity (14) in healthy individuals. In a controlled cross-over trial in 11 overweight or obese adults, consumption of a diet rich in whole grains for six weeks lowered several clinical measures of insulin resistance compared with a diet high in refined grains (15). However, in a recent randomized controlled study of 61 adults with metabolic syndrome, the consumption of a diet based on several whole-grain cereal products for 12 weeks had no effect on fasting plasma concentrations of glucose, insulin, lipids, or on insulin resistance compared with a refined grain-based diet. Yet, postprandial plasma insulin and triglycerides — but not postprandial plasma glucose — were significantly reduced with the whole grain-based diet (16). A decreased postprandial insulin response may be associated with an increase in tissue sensitivity to insulin (3). In another intervention trial in 20 healthy volunteers, three-day consumption of whole barley-based bread induced a lower insulin peak value following a standard breakfast than the same course with refined wheat bread. Whole barley-based bread consumption was also associated with an increase in circulating concentrations of gut-related hormones (e.g., peptide YY, glucagon-like peptide) and a higher gut fermentation activity. This suggested improvements in hormonal control of digestion and in colonic fermentation of resistant starch (indigestible fiber) (17), possibly promoting the feeling of satiety (18) and increasing insulin sensitivity (19).
Whole-grain consumption might be improving insulin sensitivity rather than blunting postprandial hyperglycemia; however, well-designed, large randomized controlled trials are necessary to provide further insight into how whole-grain consumption may protect against type 2 diabetes.
A meta-analysis of 10 large prospective cohort studies published between 1998 and 2010 found that the highest intake of whole grains (about three servings daily) was associated with an overall 21% reduced risk of cardiovascular disease (CVD), including coronary heart disease (CHD), ischemic heart disease, heart failure, and ischemic stroke, when compared to the lowest intake of whole grains and after adjustment for several CVD risk factors (20). Further, although evidence is currently limited, whole-grain intake may be associated with a reduced risk of hypertension, a risk factor for cardiovascular disease (21, 22).
Compared to refined grains, whole grains are rich in nutrients associated with cardiovascular risk reduction. In the Health Professionals Follow-up Study (HPFS) in 42,850 men, the top versus bottom quintile (49.6 g/day vs. 3.3 g/day) of whole-grain intake was associated with a 16% reduced risk of CHD after multiple adjustments for age, gender, and CHD risk factors (23). Further adjustments for whole-grain constituents, such as fiber, folate, magnesium, manganese, vitamin B6 and vitamin E, attenuated the association such that it was no longer statistically significant, suggesting that the micronutrient and fiber content may explain the cardiovascular benefits of consuming whole grains. Protective cardiovascular effects associated with higher intakes of whole grains and lower intakes of refined grains have included improvements in blood lipid profiles and reductions in markers of subclinical inflammation.
A meta-analysis of 21 randomized controlled trials indicated that whole-grain interventions for 4 to 16 weeks could improve an individual’s blood concentrations of fasting glucose, insulin, total and LDL-cholesterol, as well as reduce diastolic and systolic blood pressure (20). Consistent with this, a recently updated meta-analysis of 23 randomized controlled trials published between 1988 and 2015 indicated that consumption of whole grains (28 g/day-213 g/day for 2 to 16 weeks), especially whole-grain oats in cereal and other products, for a couple of weeks resulted in significant reductions in blood concentrations of triglycerides and total and LDL-cholesterol when compared to control diets with refined grain (24). Interventions that included mixed whole-grain products (bread, muesli, ready-to-eat cereal, pasta, rice, crisps, muffins, cookies) also improved blood HDL-cholesterol concentrations (24). In addition, although wheat fiber has not been found to lower serum cholesterol concentrations, numerous clinical studies have demonstrated that increasing intakes of oat fiber and soluble fiber from barley resulted in modest reductions in total and LDL-cholesterol (25-27). In light of such findings, the US Food and Drug Administration (FDA) approved claims regarding whole grains and reduction in risk of CHD that apply to diets low in saturated fat and cholesterol providing at least 3 g/day of β-glucan soluble fiber from oats (oat bran, rolled oats [oatmeal], whole oat flour) or whole-grain barley (28). Whole grains are also sources of phytosterols — compounds that can decrease serum cholesterol by interfering with its intestinal absorption (2).
Evidence from observational studies suggested an inverse association between whole-grain intake and chronic low-grade inflammation that characterizes cardiovascular and metabolic diseases (29). However, intervention studies have provided mixed results. In a recent cross-over trial in healthy low whole-grain consumers, the effect of increased consumption of mixed whole grains (mean intake, 168 g/day) for six weeks was compared to whole-grain consumption of less than 16 g/day. Increasing whole-grain intake had no effect on absolute counts of immune cells in blood (leukocytes, lymphocytes, natural killer cells), on ex vivo phagocytic activities of these cells, or on markers of inflammation (e.g., IL-10, TNF-α, C-reactive protein [CRP]) in blood (30). Previous randomized controlled studies in healthy normal weight, overweight, or obese subjects have also failed to demonstrate any benefits of whole-grain intake on markers of inflammation (31-35). One eight-week dietary intervention study in 80 overweight or obese subjects found that replacement of refined products in the habitual diet by whole-grain wheat products resulted in a significant reduction in pro-inflammatory cytokine TNF-α, a transient increase in anti-inflammatory IL-10, and no change in CRP compared to intake of refined wheat (36). In another randomized cross-over intervention study, overweight/obese children (ages, 8-15 years) were provided with a list of whole-grain products and asked to either obtain half of their grain servings from whole-grain foods every day for six weeks (whole-grain group) or abstain from consuming any of these foods (control group). Mean daily consumption of 98 g of whole-grain products (compared to 11 g/day) resulted in reductions in serum concentrations of CRP, sICAM-1 (soluble intercellular adhesion molecule-1), acute phase protein SAA (serum amyloid A), and leptin (37). An increased whole-grain intake to about five daily servings (compared to <1 serving/day) also reduced blood concentrations of CRP but had no effect on IL-10 and TNF-α concentrations in obese adults with metabolic syndrome following a hypocaloric diet (38). Inconsistency among studies may be attributed to differences in the health status of participants, the duration of interventions, and/or the types of whole grains selected. In particular, if foods with a low glycemic index (GI) can lower cardiometabolic and inflammation markers (39), substituting refined grain products by whole grains with high GI may not demonstrate any benefits regarding the risk of heart disease.
Although the protective effects of whole grains against various types of cancer are not as well established as those against type 2 diabetes mellitus and cardiovascular disease, numerous case-control studies have found inverse associations between whole-grain intake and cancer risk (40-42). An early meta-analysis of 40 case-control studies examining 20 different types of cancer found that people with higher whole-grain intakes had an overall risk of cancer that was 34% lower than those with lesser whole-grain intakes (40). Higher intakes of whole grains were most consistently associated with decreased risk of gastrointestinal tract cancers, including cancers of the mouth, throat, esophagus, stomach, colon, and rectum. A prospective cohort study that followed more than 61,000 Swedish women for 15 years found that those who consumed more than 4.5 servings of whole grains daily had a 35% lower risk of colon cancer than those who consumed less than 1.5 servings of whole grains daily (43). In the large National Institutes of Health (NIH)-AARP Diet and Health prospective study in 291,988 men and 197,623 women, mean whole-grain intakes — much lower than in the above-mentioned Swedish cohort — were also inversely associated with risk of colorectal cancer, especially rectal cancer (44). Specifically, the highest versus lowest quintile of whole-grain intake (2.6 servings/day vs. 0.4 servings/day) was associated with a 36% lower risk of developing rectal cancer (44). In a nested case-control study, including participants of the multicenter European Prospective Investigation into Cancer and Nutrition (EPIC), the top versus bottom quartile of plasma alkylresorcinol concentrations, used as a surrogate marker of whole-grain wheat and rye intakes, was found to be associated with a 52% lower incidence of distal colon cancer. No correlations were reported with the incidence of rectal cancer, colon cancer, and proximal colon cancer, or with the overall incidence of colorectal cancers (45). Not all cohort studies have suggested that whole grains might protect against intestinal cancers (46, 47). However, a dose-response analysis based on the results of six cohort studies found a 17% reduction in colorectal cancer risk with an increment of three servings (three oz-eq or 90 g) of whole grains daily (48). Of note, a recent analysis of three Scandinavian cohorts that are also part of the EPIC study and include over 110,000 participants showed an inverse correlation between total whole-grain intake and esophageal cancer risk. Each 10 g-increase in whole-grain wheat intake was found to be associated with a 50% lower risk of esophageal cancer. Such an association was not observed with whole-grain rye or with whole-grain oats (49).
In contrast to refined-grain products, whole grains are rich in numerous compounds that may be protective against cancer, particularly cancers of the gastrointestinal tract (50). Whole grains are a major source of fiber, and high-fiber intakes are thought to speed up the passage of stool through the colon, allowing less time for potentially carcinogenic compounds to stay in contact with cells that line the inner surface of the colon (51). Dietary fiber can also exert chemopreventive effects via short-chain fatty acids that are generated when fiber is fermented by the colonic microbiota (52). Whole grains also contain compounds such as phenolic acids, lignans, phytoestrogens, flavonoids, and vitamin E, that may modify signal transduction pathways that promote the development of cancer or bind potentially damaging free metal ions in the gastrointestinal tract (53, 54).
Recent large prospective cohort studies have investigated the relationship between whole-grain consumption and the risk of all-cause and cause-specific mortality. Higher versus lower intakes of whole grains (1.20 oz-eq/day versus 0.13 oz-eq/day) have been associated with a 17% lower risk of all-cause mortality in the NIH-AARP Diet and Health Study of 367,442 older adults (55). Higher whole-grain intakes were significantly associated with a decreased risk of mortality from cardiovascular disease (-17%), cancer (-15%), type 2 diabetes mellitus (-48%), respiratory disease (-11%), and infections (-23%). These associations were largely attenuated after adjustments for cereal fiber intakes, suggesting a major role for fiber in the protective effects of whole grains on mortality (55). Another recent analysis of two US prospective cohort studies, the Nurses’ Health Study (NHS) in 74,341 women and the Health Professionals Follow-up Study (HPFS) in 43,744 men, reported a 9% lower risk of all-cause mortality in individuals in the highest versus lowest quintile of whole-grain intake (56). Higher whole-grain consumption was associated with a 15% lower risk of cardiovascular disease-related mortality, but no correlation was found with cancer-related mortality. Finally, the association of whole-grain intake with mortality was also examined in over 110,000 participants of the Scandinavian HELGA cohort (57). In this cohort, a doubling of the consumption of whole-grain products or that of specific whole-grain wheat, rye, or oats was associated with a reduced risk of all-cause and cause-specific mortality.
These results from cohort studies in the US and northern Europe consistently suggested a role of whole-grain consumption in the prevention of early death.
Diets rich in whole grains and fiber may help prevent or improve constipation symptoms by softening and adding bulk to stool and by speeding its passage through the colon (58, 59). Such diets are also associated with decreased risk of diverticulosis, a condition characterized by the formation of small pouches (diverticula) in the colon. Although most people with diverticulosis experience no symptoms, about 10%-25% may develop pain or inflammation, known as diverticulitis (58). Diverticulitis was virtually unheard of before the practice of milling (refining) flour began in industrialized countries, and the role of a low-fiber diet in the development of diverticular disease is well established (60). If high-fiber diets reduce the risk of diverticular disease (61, 62), then the source of fiber (e.g., from cereal, fruit, vegetables) may be important. Interestingly, a 5 g-increase in intake of fiber from cereal was found to be associated with a 14% reduced risk of diverticular disease in a UK-based cohort of 690,075 women (mean age, 60 years) followed for up to six years; the risk of diverticular disease was decreased by 15% and 5% with a 5 g-increase in the consumption of fruit fiber and vegetable fiber, respectively (62). High-fiber diets are also recommended for people with diverticulosis in order to prevent the formation of additional diverticula rather than to resolve formed diverticula (58). People with diverticulosis are sometimes advised to avoid eating small seeds and husks to prevent them from becoming lodged in diverticula and causing diverticulitis, especially if they do not consume a high-fiber diet (58). However, it should be noted that no study has ever shown that avoiding seeds or popcorn reduces the risk of diverticulitis in an individual with diverticulosis (60).
Prospective cohort studies have consistently suggested that whole-grain consumption is associated with lower body mass index (BMI) and lower risks of weight gain and obesity (6, 20). However, a recent meta-analysis of randomized controlled trials published between 1988 and 2012 reported no significant effects of whole-grain intakes (from 18.2 g/day-150 g/day for 2 to 16 weeks) on body weight (26 trials), body fat (7 studies), and waist circumference (9 studies) in up to 2,060 normal-weight or overweight/obese adults without chronic health conditions (63). In a recent randomized, open-label, controlled trial in 60 overweight/obese individuals with metabolic syndrome, the consumption of whole grains (about 6-12 servings/day) was compared to that of refined grains during a 12-week intervention period that included a weight-maintenance diet for the first six weeks followed by six weeks of a hypocaloric diet (64). Increased whole-grain intake failed to lower body weight, BMI, percentage of body fat, or waist circumference beyond reductions also observed with consumption of refined grains. Of note, individuals who consumed whole grains showed an improved fasting glycemia compared to those fed refined grains, but other cardiometabolic variables remained unchanged (64). These results contrast with other energy-restricted dietary interventions showing a more favorable effect of whole grains on percentage of body fat compared to refined grains (38, 65). Further investigation is warranted to clarify whether whole-grain consumption could play a role in body weight regulation.
Whole-grain intakes approaching three servings daily are associated with significant reductions in chronic disease risk in populations with relatively low whole-grain intakes. The 2015-2020 Dietary Guidelines for Americans — issued jointly by the US Department of Health and Human Services and US Department of Agriculture — recommend that at least half of all grains consumed be whole grains and to increase whole-grain intake by replacing refined grains with whole grains (66). In the 2015-2020 Dietary Guidelines for Americans, the unit of measure of a whole-grain serving size is the ounce-equivalent (oz-eq). A whole-grain serving size corresponds to (1) one ounce (~30 g) of a 100% whole-grain food in its ready-to-eat form, (2) two ounces of partly whole-grain products, or (3) the amount of food containing 16 g of whole-grain ingredients (67). Table 1 summarizes the 2015-2020 US Dietary Guidelines for whole-grain intakes.
| Life Stage | Age | Daily Intake (oz-eq/day)3 | Daily Intake (g/day)4 |
|---|---|---|---|
| Children | 2-3 years | 1.5-2.5 | 24-40 |
| Children | 4-8 years | 2-3 | 32-48 |
| Children | 9-13 years | 2.5-4.5 | 40-72 |
| Adolescents | 14-18 years | 3-5 | 48-80 |
| Adults | 19 years and older | 3-5 | 48-80 |
|
1Dietary guidelines apply when no quantitative Dietary Reference Intake (DRI) value is available. |
|||
The US National Health and Nutrition Examination Survey (NHANES) 2009-2010 reported mean whole-grain intakes of 0.57 oz-eq/day in children and adolescents and 0.82 oz-eq/day in adults (68). Approximately 40% of Americans consume no whole grains, and only 2.9% of children/adolescents and 7.7% of adults consume ≥3 oz-eq/day of whole grains (68). In view of the potential health benefits of increasing whole-grain intake, three daily servings of whole-grain foods should be seen as a minimum amount, and whole-grain foods should be substituted for refined carbohydrates whenever possible.
Whole-grain foods may contain amaranth, whole-grain barley, brown and wild rice, buckwheat (kasha), millet, oats, popcorn, quinoa, whole rye, triticale, whole wheat (wheat berries) with various wheat species (including common wheat, emmer, spelt, and khorasan) (69). Unfortunately, it is not always clear from the label whether a product is made mostly from whole grains or refined grains. Some strategies to use when shopping for whole-grain foods include:
Whole grains are a source of numerous biologically active components; some are listed in Table 2.
| Macronutrients | Vitamins | Minerals | Phytochemicals |
|---|---|---|---|
| Unsaturated Fats | Folate | Magnesium | Fiber |
| Vitamin E | Potassium | Flavonoids | |
| Selenium | Lignans | ||
| Phytosterols |
Originally written in 2003 by:
Jane Higdon, Ph.D.
Linus Pauling Institute
Oregon State University
Updated in December 2005 by:
Jane Higdon, Ph.D.
Linus Pauling Institute
Oregon State University
Updated in May 2009 by:
Victoria J. Drake, Ph.D.
Linus Pauling Institute
Oregon State University
Updated in January 2016 by:
Barbara Delage, Ph.D.
Linus Pauling Institute
Oregon State University
Reviewed in January 2016 by:
Simin Liu, M.D., M.S., M.P.H., Sc.D.
Professor of Epidemiology, Professor of Medicine
Brown University
Copyright 2003-2024 Linus Pauling Institute
1. US Department of Agriculture and US Department of Health and Human Services. Dietary Guidelines for Americans 2010; 2010.
2. Bartlomiej S, Justyna RK, Ewa N. Bioactive compounds in cereal grains - occurrence, structure, technological significance and nutritional benefits - a review. Food Sci Technol Int. 2012;18(6):559-568. (PubMed)
3. Seal CJ, Brownlee IA. Whole-grain foods and chronic disease: evidence from epidemiological and intervention studies. Proc Nutr Soc. 2015;74(3):313-319. (PubMed)
4. US Food and Drug Administration. Guidance for industry: a food labeling guide. Center for Food Safety and Applied Nutrition, Office of Food Labeling [Web page]. August 2015. http://www.fda.gov/Food/GuidanceRegulation/GuidanceDocumentsRegulatoryInformation/LabelingNutrition/ucm064919.htm. Accessed 11/25/15.
5. Ferruzzi MG, Jonnalagadda SS, Liu S, et al. Developing a standard definition of whole-grain foods for dietary recommendations: summary report of a multidisciplinary expert roundtable discussion. Adv Nutr. 2014;5(2):164-176. (PubMed)
6. Cho SS, Qi L, Fahey GC, Jr., Klurfeld DM. Consumption of cereal fiber, mixtures of whole grains and bran, and whole grains and risk reduction in type 2 diabetes, obesity, and cardiovascular disease. Am J Clin Nutr. 2013;98(2):594-619. (PubMed)
7. Aune D, Norat T, Romundstad P, Vatten LJ. Whole grain and refined grain consumption and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis of cohort studies. Eur J Epidemiol. 2013;28(11):845-858. (PubMed)
8. Sun Q, Spiegelman D, van Dam RM, et al. White rice, brown rice, and risk of type 2 diabetes in US men and women. Arch Intern Med. 2010;170(11):961-969. (PubMed)
9. Blaak EE, Antoine JM, Benton D, et al. Impact of postprandial glycaemia on health and prevention of disease. Obes Rev. 2012;13(10):923-984. (PubMed)
10. Liu S. Intake of refined carbohydrates and whole grain foods in relation to risk of type 2 diabetes mellitus and coronary heart disease. J Am Coll Nutr. 2002;21(4):298-306. (PubMed)
11. Atkinson FS, Foster-Powell K, Brand-Miller JC. International tables of glycemic index and glycemic load values: 2008. Diabetes Care. 2008;31(12):2281-2283. (PubMed)
12. Augustin LS, Kendall CW, Jenkins DJ, et al. Glycemic index, glycemic load and glycemic response: An International Scientific Consensus Summit from the International Carbohydrate Quality Consortium (ICQC). Nutr Metab Cardiovasc Dis. 2015;25(9):795-815. (PubMed)
13. McKeown NM, Meigs JB, Liu S, Wilson PW, Jacques PF. Whole-grain intake is favorably associated with metabolic risk factors for type 2 diabetes and cardiovascular disease in the Framingham Offspring Study. Am J Clin Nutr. 2002;76(2):390-398. (PubMed)
14. Liese AD, Roach AK, Sparks KC, Marquart L, D'Agostino RB, Jr., Mayer-Davis EJ. Whole-grain intake and insulin sensitivity: the Insulin Resistance Atherosclerosis Study. Am J Clin Nutr. 2003;78(5):965-971. (PubMed)
15. Pereira MA, Jacobs DR, Jr., Pins JJ, et al. Effect of whole grains on insulin sensitivity in overweight hyperinsulinemic adults. Am J Clin Nutr. 2002;75(5):848-855. (PubMed)
16. Giacco R, Costabile G, Della Pepa G, et al. A whole-grain cereal-based diet lowers postprandial plasma insulin and triglyceride levels in individuals with metabolic syndrome. Nutr Metab Cardiovasc Dis. 2014;24(8):837-844. (PubMed)
17. Nilsson AC, Johansson-Boll EV, Bjorck IM. Increased gut hormones and insulin sensitivity index following a 3-d intervention with a barley kernel-based product: a randomised cross-over study in healthy middle-aged subjects. Br J Nutr. 2015;114(6):899-907. (PubMed)
18. Rosen LA, Ostman EM, Bjorck IM. Effects of cereal breakfasts on postprandial glucose, appetite regulation and voluntary energy intake at a subsequent standardized lunch; focusing on rye products. Nutr J. 2011;10:7. (PubMed)
19. Robertson MD, Bickerton AS, Dennis AL, Vidal H, Frayn KN. Insulin-sensitizing effects of dietary resistant starch and effects on skeletal muscle and adipose tissue metabolism. Am J Clin Nutr. 2005;82(3):559-567. (PubMed)
20. Ye EQ, Chacko SA, Chou EL, Kugizaki M, Liu S. Greater whole-grain intake is associated with lower risk of type 2 diabetes, cardiovascular disease, and weight gain. J Nutr. 2012;142(7):1304-1313. (PubMed)
21. Wang L, Gaziano JM, Liu S, Manson JE, Buring JE, Sesso HD. Whole- and refined-grain intakes and the risk of hypertension in women. Am J Clin Nutr. 2007;86(2):472-479. (PubMed)
22. Flint AJ, Hu FB, Glynn RJ, et al. Whole grains and incident hypertension in men. Am J Clin Nutr. 2009;90(3):493-498. (PubMed)
23. Jensen MK, Koh-Banerjee P, Hu FB, et al. Intakes of whole grains, bran, and germ and the risk of coronary heart disease in men. Am J Clin Nutr. 2004;80(6):1492-1499. (PubMed)
24. Hollaender PL, Ross AB, Kristensen M. Whole-grain and blood lipid changes in apparently healthy adults: a systematic review and meta-analysis of randomized controlled studies. Am J Clin Nutr. 2015;102(3):556-572. (PubMed)
25. Ames NP, Rhymer CR. Issues surrounding health claims for barley. J Nutr. 2008;138(6):1237S-1243S. (PubMed)
26. Behall KM, Scholfield DJ, Hallfrisch J. Diets containing barley significantly reduce lipids in mildly hypercholesterolemic men and women. Am J Clin Nutr. 2004;80(5):1185-1193. (PubMed)
27. Truswell AS. Cereal grains and coronary heart disease. Eur J Clin Nutr. 2002;56(1):1-14. (PubMed)
28. U.S. Food and Drug Administration. CFR - Code of Federal Regulations Title 21, Vol. 2. Part 101: food labeling. Subpart E: specific requirements for health claims.
29. Lefevre M, Jonnalagadda S. Effect of whole grains on markers of subclinical inflammation. Nutr Rev. 2012;70(7):387-396. (PubMed)
30. Ampatzoglou A, Williams CL, Atwal KK, et al. Effects of increased wholegrain consumption on immune and inflammatory markers in healthy low habitual wholegrain consumers. Eur J Nutr. 2015. Jan 25. [Epub ahead of print]. (PubMed)
31. Andersson A, Tengblad S, Karlstrom B, et al. Whole-grain foods do not affect insulin sensitivity or markers of lipid peroxidation and inflammation in healthy, moderately overweight subjects. J Nutr. 2007;137(6):1401-1407. (PubMed)
32. Brownlee IA, Moore C, Chatfield M, et al. Markers of cardiovascular risk are not changed by increased whole-grain intake: the WHOLEheart study, a randomised, controlled dietary intervention. Br J Nutr. 2010;104(1):125-134. (PubMed)
33. Giacco R, Clemente G, Cipriano D, et al. Effects of the regular consumption of wholemeal wheat foods on cardiovascular risk factors in healthy people. Nutr Metab Cardiovasc Dis. 2010;20(3):186-194. (PubMed)
34. Nelson K, Mathai ML, Ashton JF, et al. Effects of malted and non-malted whole-grain wheat on metabolic and inflammatory biomarkers in overweight/obese adults: A randomised crossover pilot study. Food Chem. 2016;194:495-502. (PubMed)
35. Tighe P, Duthie G, Vaughan N, et al. Effect of increased consumption of whole-grain foods on blood pressure and other cardiovascular risk markers in healthy middle-aged persons: a randomized controlled trial. Am J Clin Nutr. 2010;92(4):733-740. (PubMed)
36. Vitaglione P, Mennella I, Ferracane R, et al. Whole-grain wheat consumption reduces inflammation in a randomized controlled trial on overweight and obese subjects with unhealthy dietary and lifestyle behaviors: role of polyphenols bound to cereal dietary fiber. Am J Clin Nutr. 2015;101(2):251-261. (PubMed)
37. Hajihashemi P, Azadbakht L, Hashemipor M, Kelishadi R, Esmaillzadeh A. Whole-grain intake favorably affects markers of systemic inflammation in obese children: a randomized controlled crossover clinical trial. Mol Nutr Food Res. 2014;58(6):1301-1308. (PubMed)
38. Katcher HI, Legro RS, Kunselman AR, et al. The effects of a whole grain-enriched hypocaloric diet on cardiovascular disease risk factors in men and women with metabolic syndrome. Am J Clin Nutr. 2008;87(1):79-90. (PubMed)
39. Feliciano Pereira P, das Gracas de Almeida C, Alfenas Rde C. Glycemic index role on visceral obesity, subclinical inflammation and associated chronic diseases. Nutr Hosp. 2014;30(2):237-243. (PubMed)
40. Jacobs DR, Jr., Marquart L, Slavin J, Kushi LH. Whole-grain intake and cancer: an expanded review and meta-analysis. Nutr Cancer. 1998;30(2):85-96. (PubMed)
41. La Vecchia C, Chatenoud L, Negri E, Franceschi S. Session: Whole cereal grains, fibre and human cancer Wholegrain cereals and cancer in Italy. Proc Nutr Soc. 2003;62(1):45-49. (PubMed)
42. Chan JM, Wang F, Holly EA. Whole grains and risk of pancreatic cancer in a large population-based case-control study in the San Francisco Bay Area, California. Am J Epidemiol. 2007;166(10):1174-1185. (PubMed)
43. Larsson SC, Giovannucci E, Bergkvist L, Wolk A. Whole grain consumption and risk of colorectal cancer: a population-based cohort of 60,000 women. Br J Cancer. 2005;92(9):1803-1807. (PubMed)
44. Schatzkin A, Mouw T, Park Y, et al. Dietary fiber and whole-grain consumption in relation to colorectal cancer in the NIH-AARP Diet and Health Study. Am J Clin Nutr. 2007;85(5):1353-1360. (PubMed)
45. Kyro C, Olsen A, Landberg R, et al. Plasma alkylresorcinols, biomarkers of whole-grain wheat and rye intake, and incidence of colorectal cancer. J Natl Cancer Inst. 2014;106(1):djt352. (PubMed)
46. McCullough ML, Robertson AS, Chao A, et al. A prospective study of whole grains, fruits, vegetables and colon cancer risk. Cancer Causes Control. 2003;14(10):959-970. (PubMed)
47. Pietinen P, Malila N, Virtanen M, et al. Diet and risk of colorectal cancer in a cohort of Finnish men. Cancer Causes Control. 1999;10(5):387-396. (PubMed)
48. Aune D, Chan DS, Lau R, et al. Dietary fibre, whole grains, and risk of colorectal cancer: systematic review and dose-response meta-analysis of prospective studies. BMJ. 2011;343:d6617. (PubMed)
49. Skeie G, Braaten T, Olsen A, et al. Intake of whole grains and incidence of oesophageal cancer in the HELGA Cohort. Eur J Epidemiol. 2015. Jun 20. [Epub ahead of print]. (PubMed)
50. Slavin JL. Mechanisms for the impact of whole grain foods on cancer risk. J Am Coll Nutr. 2000;19(3 Suppl):300S-307S. (PubMed)
51. Lipkin M, Reddy B, Newmark H, Lamprecht SA. Dietary factors in human colorectal cancer. Annu Rev Nutr. 1999;19:545-586. (PubMed)
52. Scharlau D, Borowicki A, Habermann N, et al. Mechanisms of primary cancer prevention by butyrate and other products formed during gut flora-mediated fermentation of dietary fibre. Mutat Res. 2009;682(1):39-53. (PubMed)
53. Kuijsten A, Arts IC, Hollman PC, van't Veer P, Kampman E. Plasma enterolignans are associated with lower colorectal adenoma risk. Cancer Epidemiol Biomarkers Prev. 2006;15(6):1132-1136. (PubMed)
54. Van Hung P. Phenolic Compounds of Cereals and Their Antioxidant Capacity. Crit Rev Food Sci Nutr. 2016;56(1):25-35. (PubMed)
55. Huang T, Xu M, Lee A, Cho S, Qi L. Consumption of whole grains and cereal fiber and total and cause-specific mortality: prospective analysis of 367,442 individuals. BMC Med. 2015;13:59. (PubMed)
56. Wu H, Flint AJ, Qi Q, et al. Association between dietary whole grain intake and risk of mortality: two large prospective studies in US men and women. JAMA Intern Med. 2015;175(3):373-384. (PubMed)
57. Johnsen NF, Frederiksen K, Christensen J, et al. Whole-grain products and whole-grain types are associated with lower all-cause and cause-specific mortality in the Scandinavian HELGA cohort. Br J Nutr. 2015;114(4):608-623. (PubMed)
58. Slavin JL. Position of the American Dietetic Association: health implications of dietary fiber. J Am Diet Assoc. 2008;108(10):1716-1731. (PubMed)
59. Woo HI, Kwak SH, Lee Y, Choi JH, Cho YM, Om AS. A Controlled, Randomized, Double-blind Trial to Evaluate the Effect of Vegetables and Whole Grain Powder That Is Rich in Dietary Fibers on Bowel Functions and Defecation in Constipated Young Adults. J Cancer Prev. 2015;20(1):64-69. (PubMed)
60. Farrell RJ, Farrell JJ, Morrin MM. Diverticular disease in the elderly. Gastroenterol Clin North Am. 2001;30(2):475-496. (PubMed)
61. Crowe FL, Appleby PN, Allen NE, Key TJ. Diet and risk of diverticular disease in Oxford cohort of European Prospective Investigation into Cancer and Nutrition (EPIC): prospective study of British vegetarians and non-vegetarians. BMJ. 2011;343:d4131. (PubMed)
62. Crowe FL, Balkwill A, Cairns BJ, et al. Source of dietary fibre and diverticular disease incidence: a prospective study of UK women. Gut. 2014;63(9):1450-1456. (PubMed)
63. Pol K, Christensen R, Bartels EM, Raben A, Tetens I, Kristensen M. Whole grain and body weight changes in apparently healthy adults: a systematic review and meta-analysis of randomized controlled studies. Am J Clin Nutr. 2013;98(4):872-884. (PubMed)
64. Harris Jackson K, West SG, Vanden Heuvel JP, et al. Effects of whole and refined grains in a weight-loss diet on markers of metabolic syndrome in individuals with increased waist circumference: a randomized controlled-feeding trial. Am J Clin Nutr. 2014;100(2):577-586. (PubMed)
65. Kristensen M, Toubro S, Jensen MG, et al. Whole grain compared with refined wheat decreases the percentage of body fat following a 12-week, energy-restricted dietary intervention in postmenopausal women. J Nutr. 2012;142(4):710-716. (PubMed)
66. US Department of Health and Human Services and US Department of Agriculture. 2015 – 2020 Dietary Guidelines for Americans. 8th ed; 2015. Available at: http://health.gov/dietaryguidelines/2015/guidelines/.
67. Whole Grains Council. What is an Ounce Equivalent? Available at: http://wholegrainscouncil.org/whole-grains-101/what-is-an-ounce-equivalent. Accessed 11/27/15.
68. Reicks M, Jonnalagadda S, Albertson AM, Joshi N. Total dietary fiber intakes in the US population are related to whole grain consumption: results from the National Health and Nutrition Examination Survey 2009 to 2010. Nutr Res. 2014;34(3):226-234. (PubMed)
69. Willett WC. Eat, Drink, and be Healthy: The Harvard Medical School Guide to Healthy Eating. New York: Simon & Schuster; 2001.