Nutrition Research
-
Macronutrients
-
Micronutrients
-
Phytochemicals
-
Lifestyle Factors
Summary
The large intestine includes the cecum, the colon, the rectum, and the anal canal. The colon is described according to four anatomic regions, from the cecum to the rectum: ascending colon, transverse colon, descending colon, and sigmoid colon. Its physiological function is to process and absorb undigested nutrients, absorb electrolytes and water, and excrete waste products via the rectum.
The intestinal epithelium is entirely renewed every three to five days. The single layer of epithelial cells is derived from immature cells that multiply in the small pits (called colonic crypts) located throughout the intestinal epithelium. Unlike the epithelium of the small intestine, the colonic epithelium is flat and does not have villi.
Colorectal cancer is the most common gastrointestinal cancer, accounting for over 1.8 million new cases per year worldwide. It is also the second leading cause of death by cancer (behind lung cancer) in the US. The development of colorectal cancer is associated with alterations of different molecular processes driving the transformation of normal cells into cancer cells. These alterations may be almost entirely caused by inherited genetic mutations as in individuals with familial adenomatous polyposis or by modifiable lifestyle factors and chronic inflammation in cases of non-hereditary (sporadic) colorectal cancer.
DEFINITIONS
Anal canal - the most terminal portion of the large intestine, between the rectum and the anus
Cecum - the first part of the large intestine, connecting the small intestine with the ascending colon
Colonic crypts - invaginations that open into the surface epithelium. Stem cells in the lowest (basal) part of crypts multiply and acquire specific functions, thereby ensuring the renewal of mature epithelial cells.
Electrolytes - charged particles (called ions) that are constituents of all living cells and tissues. Major electrolytes in the body include sodium, potassium, magnesium, calcium, chloride, bicarbonate, and phosphate.
Familial adenomatous polyposis - a hereditary syndrome characterized by the formation of many polyps in the colon and the rectum. Some of the colorectal polyps (adenomas) may become cancerous.
Polyps - a benign (non-cancerous) mass of cells that forms on the inside of a hollow organ, such as the colon
Rectum - the portion of the large intestine, connecting the sigmoid colon to the anal canal. The rectum stores stool until it is evacuated from the body.
Villi - small finger-like projections into the lumen of the small intestine
Disease Overview
Incidence
In 2018, over 1.8 million people worldwide received a diagnosis of colorectal cancer (1). Colorectal cancer is the third most commonly diagnosed cancer in men, after lung and prostate cancers, and the second in women, after breast cancer.
-
The disease affects more men than women: on average, 23.6 new cases per 100,000 among men versus 16.3 new cases per 100,000 among women (1).
-
The highest incidence in men (≥35.7 new cases per 100,000) and women (≥24.5 new cases per 100,000) is reported in populations of high-income countries: Europe, Australia, New Zealand, South Korea, Japan, and North America (1).
-
The incidence is rising in low- and middle-income countries as they undergo rapid societal and economic development. The incidence keeps increasing in high-income countries like Canada, UK, Denmark, and Singapore, but is decreasing in the US, Japan, and France (2).
-
In the US, colorectal cancer is most common in Blacks (42.2 new cases per 100,000) and least common is Asians/Pacific islanders (29 new cases per 100,000) (3).
DEFINITION
Incidence - proportion of new cases of a disease in a given population at risk over a specific period of time
Adenoma-carcinoma sequence
The adenoma-carcinoma sequence describes the development of colorectal cancer from normal epithelium to carcinoma with the concomitant accumulation of epigenetic and genetic anomalies (4).
Colorectal adenomas (also called adenomatous polyps) are considered to be precursor lesions for most cases of colorectal cancer within the adenoma-carcinoma sequence. For a subtype of colorectal cancer called serrated adenocarcinoma, the early lesions are sessile serrated polyps rather than adenomatous polyps.
DEFINITIONS
Adenoma - benign tumor of glandular tissue like the colorectal mucosa. The terms adenoma, adenomatous polyp, and polyp are often used interchangeably
Carcinoma - a type of malignant tumor (cancer) of epithelial origin. Adenocarcinoma is a subtype of carcinoma that developed from glandular tissue. Most colorectal cancers are adenocarcinomas
Epigenetic anomalies - refers to anomalies that do not involve alterations of the DNA sequence, as opposed to genetic anomalies, e.g., abnormal DNA methylation
Classification
Most colorectal cancers are adenocarcinomas. They can be classified according to molecular subtype; this helps stratify patients into good and poor prognosis groups and personalize treatment options (5, 6).
DEFINITION
Adenocarcinoma - a type of malignant tumor derived from a benign tumor (adenoma) of glandular origin
Etiology
There is not one single cause of colorectal cancer. Instead, a number of factors, either modifiable or non-modifiable, can influence the risk of developing colorectal cancer.
Genetic factors
Hereditary colorectal cancer: About 5% of people diagnosed with colorectal cancer have inherited genetic predispositions. These genetic predispositions give rise to a number of colorectal cancer syndromes. The two most common syndromes are hereditary nonpolyposis colorectal cancer (HNPCC or Lynch syndrome) and familial adenomatous polyposis (FAP).
HNPCC is associated with mutations in genes involved in DNA repair, while FAP is associated with alterations in the specific genes, APC and MUTYH.
Familial colorectal cancer: About 15%-30% of colorectal cancer cases occur in people with a family history of colorectal adenoma/cancer.
Sporadic colorectal cancer: The large majority of colorectal cancer cases are not related to family history or inherited factors. Sporadic colorectal cancers are primarily linked to diet, lifestyle, and environmental factors, which can lead to genetic mutations and epigenetic anomalies. Several genetic pathways have been involved in the development of sporadic cases of colorectal cancer.
Inflammatory bowel disease
People experiencing ulcerative colitis or Crohn’s disease have a higher risk of colorectal cancer.
Unhealthy diets and lifestyle factors
Diet is closely associated with colorectal cancer. High intakes of fruit and vegetables, dairy products, fish, and fiber are thought to protect against colorectal cancer, while consumption of high amounts of red and processed meats is likely to increase the risk of colorectal cancer. Cigarette smoking, alcohol consumption, and physical inactivity also contribute to increasing the risk of colorectal cancer.
Other risk factors
Increasing age, male gender, and obesity are associated with a higher risk of developing colorectal cancer.
References:
Aran et al. (2016) (5)
Kuipers et al. (2015) (7)
Connell et al. (2017) (8)
Prevention and Screening
The American Cancer Society has developed recommendations, highlighting the importance of weight control, physical activity, and a healthy diet, for the primary prevention of cancer (9). Most colorectal cancer cases are connected to diet and lifestyle. Achieving and maintaining a healthy weight throughout life, being physically active, and consuming a healthy diet with an emphasis on fruit and vegetables, while limiting alcohol drinks and avoiding tobacco smoking, should lower one’s risk of developing sporadic colorectal cancer.
Screening is meant to detect early lesions in people who have no symptoms of the disease. It takes between 10 to 15 years for abnormal colorectal cells to grow into polyps. Regular screening allows the detection and removal of polyps. Additionally, detecting colorectal cancers when they are small makes them easier to treat and cure. Screening tests include stool-based tests and colonoscopy. Age-specific recommendations for cancer screening are provided by the American Cancer Society.
DEFINITION
Colonoscopy - procedure that consists of looking inside the colon and rectum with the help of a flexible instrument (colonoscope) that has a light and small video camera on the end. The colonoscope is introduced into the rectum and colon through the anus.
Nutrition Research
DEFINITIONS
Test tube (in vitro) experiment - a research experiment performed in a test tube, culture dish, or other artificial environment outside of a living organism; in vitro is a Latin phrase meaning ‘in glass’
Animal experiment - a research experiment performed in a laboratory animal; many different animal species are studied in the laboratory, including terrestrial (land), aquatic (water), and microscopic animals
Observational study - a human research study in which no experimental intervention or treatment is applied, and participants are simply observed. Observational studies include, among others, case-control and prospective cohort studies. Observational studies can be used to examine whether there may be a relationship between an exposure and an outcome, but they cannot inform whether there is a causal relationship.
Randomized controlled trial - a human research study in which participants are randomly assigned to receive an active treatment or an inert (control or placebo) treatment. Randomized controlled trials are powered to examine whether there is a cause-and-effect relationship between an exposure and an outcome. This type of study is often used to test the efficacy of an active treatment on a specific outcome compared to a control.
Placebo - a substance without therapeutic effect (i.e., a chemically inert substance)
Dietary Fat
What it does
General
-
Fat in the diet is a major source of energy for the body, providing 9 calories per gram (g).
-
Types (saturated, monounsaturated, polyunsaturated [including essential], and trans fatty acids) and amounts of fat in one’s diet have been linked to either harms or benefits to health.
-
Dietary guidelines recommend avoiding trans fat, limiting saturated fat (<10% of total energy intake), and replacing saturated fat by mono/polyunsaturated fat (10, 11).
Cancer-specific
-
In animal experiments, omega-3 fatty acids (a type of polyunsaturated fatty acids) and their derivatives reduced the risk of cancer by triggering mechanisms against inflammation, oxidative stress, and abnormal cell proliferation (12, 13).
What we know
-
Consumption of all or specific types of fatty acids from food sources is not associated with a lower or higher risk of colorectal cancer (14).
-
Fish oil or omega-3 fatty acid supplements are currently being evaluated for use as an adjunct to chemotherapy in patients with colorectal cancer. These fatty acids may increase the tolerability and/or therapeutic response to anticancer drugs (13).
DEFINITIONS
Adjunct to chemotherapy - also called add-on therapy, it refers to a treatment that is given in addition to the standard-of-care for chemotherapy in order to enhance efficacy of treatment
Chemotherapy - literally, treatment with drugs. Commonly used to describe the use of drugs in the treatment of cancer.
Oxidative stress - refers to the condition in which the effects of pro-oxidants (e.g., reactive oxygen species) exceed the ability of antioxidant systems to neutralize them
Trans fatty acids - trans, unsaturated fatty acids are naturally occurring in small amounts in meat and milk but are produced in large amounts during the industrial processing of vegetable and fish oils (hydrogenated or partially hydrogenated oils). The trans configuration of double bonds in unsaturated fatty acids contrasts with the naturally occurring cis configuration.
For references and more information, the 2015-2020 Dietary Guidelines for Americans provide detailed advice on fat consumption. Specific recommendations for essential fatty acid (omega-3 and omega-6) intake can also be found in the Essential Fatty Acids article.

Fiber
What it does
General
-
Fiber is a general term for (primarily) carbohydrates that are resistant to digestion by human enzymes.
-
Fiber may be obtained from food sources, additives, and dietary supplements.
-
As fiber travels through the digestive tract, its physical properties (which vary depending on the type of fiber ingested) impart different health effects.
-
Mechanisms by which fiber may exert health benefits on the gastrointestinal and cardiovascular systems include glycemic control, cholesterol and blood pressure lowering, and regulation of stool consistency and elimination.
Cancer-specific
-
Fiber consumption may protect the digestive tract by reducing exposure of the mucosa to carcinogens. Additionally, the fermentation of certain fibers in the large intestine releases short-chain fatty acids that have anticancer activities.
-
There is evidence showing that higher fiber intakes are associated with reduced risks of cancers of the digestive tract (in particular esophageal, gastric, colorectal, and pancreatic cancers), as well as breast and, possibly, ovarian and prostate cancers.
What we know
-
High intakes of fiber-rich foods are associated with a lower risk of colorectal cancer (15).
HIGHLIGHT
Fiber is identified as a shortfall nutrient of public health concern in the 2015-2020 Dietary Guidelines for Americans. Intake recommendations and good sources of dietary fiber can be found in the Fiber article.
Some suggestions for increasing fiber intake:
-
Eat at least five servings of fruit and vegetables daily.
-
Substitute whole grains for refined grains.
-
Eat oatmeal, whole-grain cereal, or bran cereal for breakfast.
-
Eat beans, split peas, or lentils at least once weekly.
-
Substitute nuts or popcorn for less healthful snacks like potato chips or candy.
For references and more information, see the section on colorectal cancer in the Fiber article.

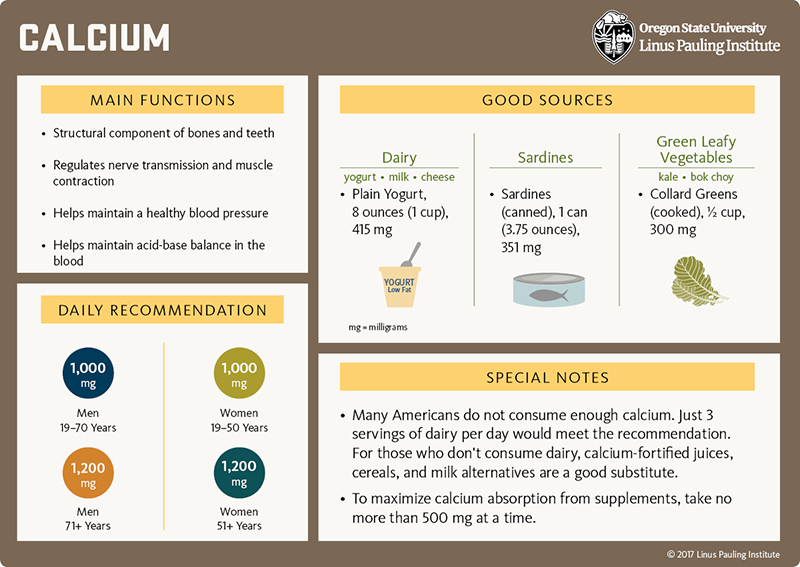
Calcium
What it does
General
-
Calcium is a major structural component of bones and teeth.
-
Calcium plays an essential role in cell-signaling pathways and is therefore fundamental to virtually all physiological functions.
-
Dairy products contribute to 75% of calcium intakes in the American diet.
Cancer-specific
-
A calcium-sensing receptor that helps maintain blood calcium within a tight concentration range is expressed throughout the intestines. This receptor is thought to be involved in the regulation of inflammatory pathways and to act as a tumor suppressor in the large intestine (16).
What we know
-
Higher intakes of calcium from food (17, 18) or supplements (18) are associated with a lower risk of colorectal cancer.
-
Specifically, a 300 mg/day increase in calcium intake — from diet or from supplements — is associated with an 8% lower risk of colorectal cancer (18).
-
Supplementation with calcium (1.2-2 g/day for up to 5 years) reduces the risk of colorectal adenomas in people with a history of colorectal adenoma or cancer (19, 20).
DEFINITIONS
Cell-signaling pathways - refers to cascades of events leading to changes within a cell in response to changes in a cell’s environment
Tumor suppressor - refers here to a protein that functions to protect cells from progressing in the path to cancer. The expression or function of tumor suppressors is often disrupted in cancer cells.
For general information about calcium, see the Calcium article.
[Download PDF]

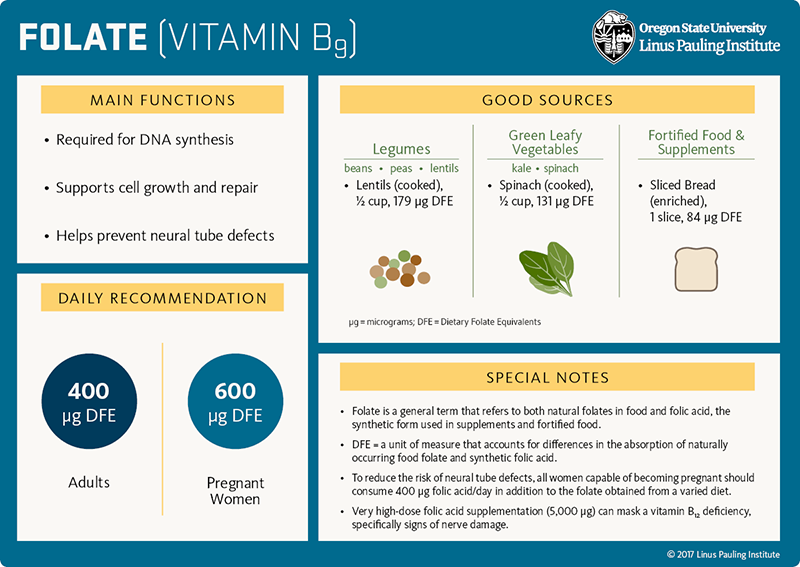
Folate
What it does
General
-
Folate is a B-vitamin that is required for DNA synthesis and the formation of new cells. The vitamin is specifically involved in the synthesis of thymine, an essential DNA component.
-
The B-vitamins folate, riboflavin, vitamin B12, and vitamin B6 work together to convert homocysteine to methionine, an amino acid important for methylation reactions and countless other cellular activities.
Cancer-specific
-
Folate deficiency may increase genomic instability and chromosome breakage, thereby contributing to cancer development.
-
Conversely, it has been argued that folate supplementation could fuel cell multiplication and thus promote cancer development. However, there is no evidence in humans that folate supplementation or consumption of fortified food increases the risk of any cancer type.
-
Anti-folate molecules that interfere with DNA synthesis are successfully used in anticancer therapies.
What we know
-
Poor folate status (21) and certain genetic variations in the metabolism of folate (22) have been associated with an increased risk of developing colorectal cancer.
-
Folic acid supplementation may protect people with low folate status against primary or recurrent colorectal tumors; e.g., people with inflammatory bowel disease who are at risk of folate deficiency may benefit from folic acid supplementation in terms of colorectal cancer prevention (23). Yet, there is no additional benefit to those who are already replete (24, 25).
-
Follow-up of a randomized controlled trial suggested than folic acid supplementation (1 mg/day) may increase the risk of sessile serrated adenomas (26).
HIGHLIGHT
Inadequate folate status in early pregnancy increases the risk of specific birth defects called
neural tube defects (NTDs). In 1998, the US mandated that all refined grain products be fortified with folic acid; this has greatly reduced the occurrence of NTDs. Worldwide, 82 other countries mandate folic acid fortification of at least one refined grain
(27).
DEFINITIONS
Methylation reaction - this type of reaction consists of adding a methyl group (-CH3) to a given substrate
Neural tube defects - birth defects arising from the improper closer of the neural tube (the precursor of the brain and spinal cord) of the embryo, which occurs in the 4th week following conception
Recurrent tumor - refers to a tumor that comes back in the same place or close by, after a period of time during which it could not be detected
Replete - having fulfilled nutrient requirements
Sessile serrated adenomas - a type of polyp that can transform into a subtype of colorectal cancer called serrated adenocarcinoma
Thymine - a base that is combined with a sugar and a phosphate group to form one of four building blocks of DNA. The other bases are adenine, guanine, and cytosine. Thymine is replaced by uracil in RNA.
For more information, see the section on colorectal cancer in the Folate article.
[Download PDF]

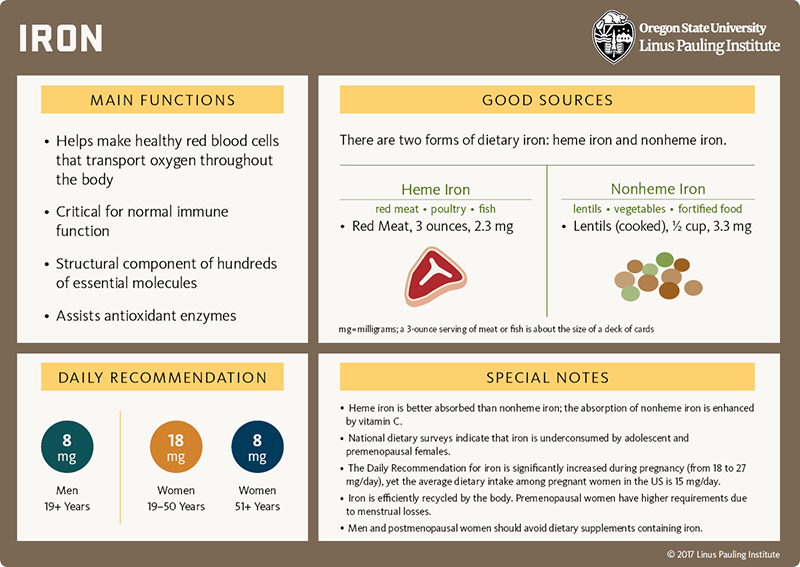
Iron
What it does
General
-
Iron is an essential component of hundreds of essential proteins involved in a wide range of activities, such as oxygen transport and storage, energy metabolism, and DNA synthesis.
-
Some of these proteins, including hemoglobin, cytochromes, and antioxidant enzymes, require iron-containing heme to carry out their biological activities.
Cancer-specific
-
Free (unbound) iron can react with hydrogen peroxide to generate hydroxyl radicals. Iron can also contribute to the formation of nitrosamines. Both types of compounds can damage DNA and increase the risk of cancer.
What we know
-
High consumption of heme iron, mainly from red meat, has been associated with a higher risk of colorectal cancer (28).
DEFINITIONS
Antioxidant enzymes - enzymes that contribute to neutralizing atoms or molecules capable of damaging essential cell constituents
Cytochromes - a family of enzymes involves in electron transfer
Electron - a stable atomic particle with a negative charge
Hydroxyl radical - a type of reactive oxygen species that can be neutralized by antioxidants
Nitrosamines - cancer-causing compounds produced from nitrites and amines derived from proteins either during meat processing or under the strongly acidic condition of the stomach
For references and more information, see the section on cancer in the Iron article.
[Download PDF]

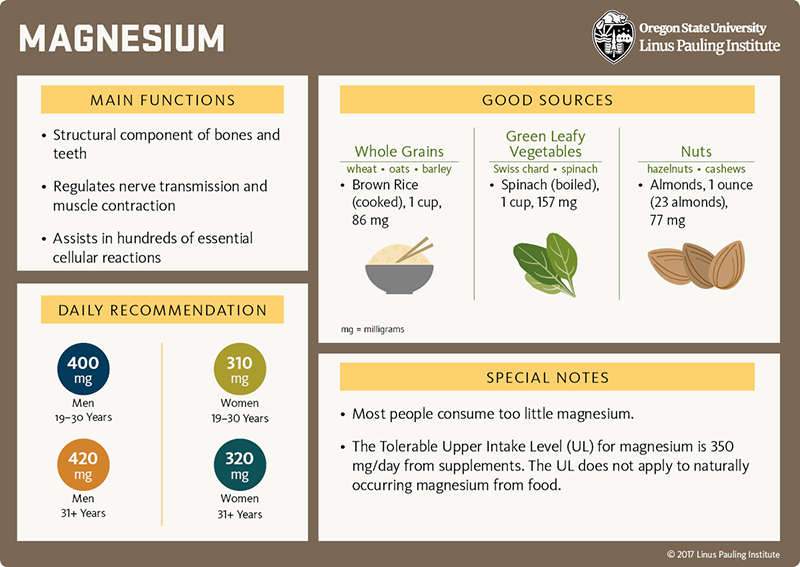
Magnesium
What it does
General
-
Magnesium is a cofactor for enzymes that catalyze hundreds of essential reactions in the metabolism of carbohydrates, fats, and proteins.
-
Magnesium is required for the synthesis of ATP, which is involved in virtually all cellular processes.
Cancer-specific
-
Magnesium binds to negatively charged molecules and has a structural role in chromosomes and cell membranes. Magnesium deficiency is thus likely to affect genome stability.
-
Magnesium is involved in key cell functions, including proliferation and migration, which are altered in cancer.
What we know
-
Higher magnesium intakes in a representative sample of the US population have been linked to lower risk of poor vitamin D status. Adequate vitamin D status is associated with a lower risk of developing colorectal cancer.
-
Higher magnesium intakes are associated with a lower risk of developing colorectal cancer (17).
DEFINITION
ATP - acronym for adenosine triphosphate; an important compound for the storage of energy in cells, as well as the synthesis of DNA
[Download PDF]

Riboflavin
What it does
General
-
Riboflavin (vitamin B2) is a water-soluble vitamin that assists several metabolic and antioxidant enzymes and helps convert food into useable energy.
-
Riboflavin is needed to convert folate to a form needed to maintain normal concentrations of homocysteine in blood and to support methylation reactions in the body.
Cancer-specific
-
Poor riboflavin status can affect folate metabolism, thereby potentially increasing the risk of cancer.
What we know
-
The available evidence is mixed regarding the potential association between higher intakes of riboflavin and lower risk of colorectal cancer (29-31).
DEFINITIONS
Antioxidant enzymes - enzymes that contribute to neutralizing atoms or molecules capable of damaging essential cell constituents
Methylation reaction - a type of reaction that consists of adding a methyl group (-CH3) to a given substrate
For more information, see the section on cancer prevention in the Riboflavin article.

[Download PDF]
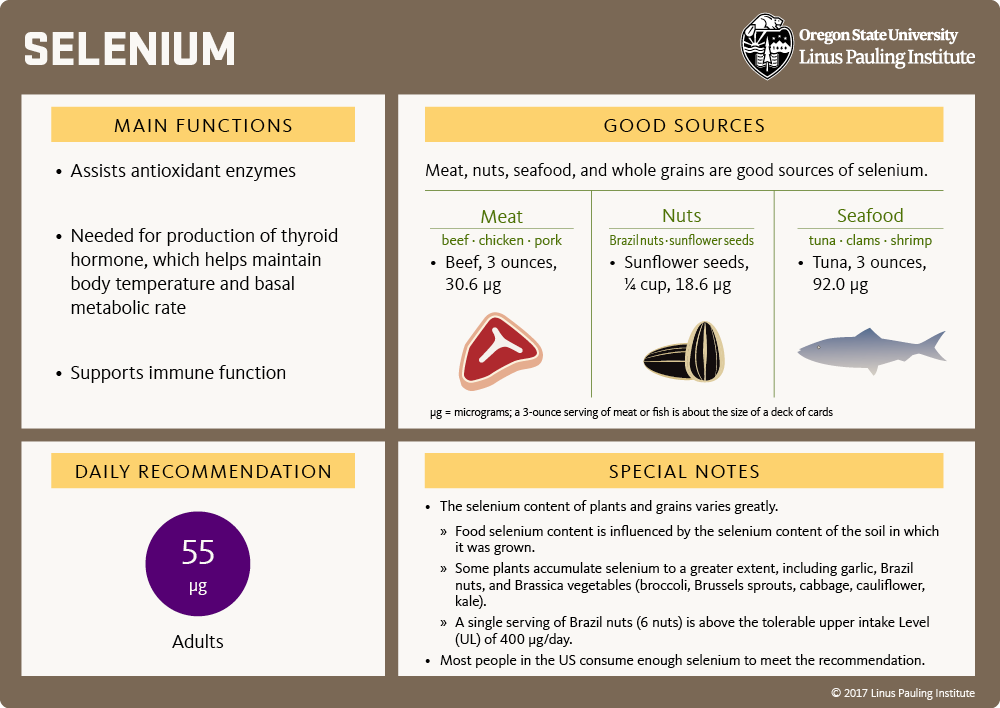
Selenium
What it does
General
-
Selenium is an essential trace mineral required for the synthesis of a particular amino acid called selenocysteine.
-
Selenocysteine is a structural component of at least 25 proteins, including enzymes involved in the making of thyroid hormones, as well as several antioxidant enzymes.
Cancer-specific
-
Deficiency in selenium might compromise antioxidant enzyme activities that protect essential cell constituents against oxidative damage. Oxidative damage to DNA in particular may play a role in the development of cancer.
-
Trials have found no benefit of selenium supplements in the prevention of total cancer, specific types of cancer, or mortality related to cancer (32).
What we know
-
Some, but not all, observational studies reported a lower risk of colorectal cancer with higher selenium intakes (from diet and supplements) or higher selenium nutritional status (32, 33).
-
In general, randomized controlled trials have not found selenium supplementation lowers risk of colorectal cancer occurrence or recurrence (see the article on Selenium).
DEFINITIONS
Antioxidant enzymes - enzymes that contribute to neutralizing atoms or molecules capable of damaging essential cell constituents
Oxidative damage - damage caused to large molecules (i.e., carbohydrates, protein, fat, DNA) by the presence of reactive oxygen species
Randomized controlled trial - a human research study in which participants are assigned by chance alone to receive either an experimental agent (the treatment group) or a placebo (the control group)
[Download PDF]

Vitamin A
What it does
General
-
Vitamin A refers to a number of fat-soluble vitamins (collectively known as retinoids) involved in the growth and differentiation of virtually all cells in the body.
-
Vitamin A is essential for normal vision, reproduction, development, and immune function.
-
Retinol is a ready-to-use form of vitamin A present in the body and food of animal origin. β-Carotene and other carotenoids in plants can be converted (to some extent) into retinol by the body (see Carotenoids below).
Cancer-specific
-
Test tube and animal experiments showed that all-trans retinoic acid — a biologically active form of vitamin A — can stop the multiplication and spread of cancer cells and trigger their death (34).
-
Several retinoids are approved for the treatment of cancers, such as neuroblastoma and certain lymphomas (35).
What we know
-
Higher intakes of vitamin A from food sources and/or supplements have not been associated with a lower risk of colorectal cancer (29, 36, 37).
HIGHLIGHT
Consumption of high doses of vitamin A (in the form of retinol or retinyl esters) can be highly toxic and is unlikely to reduce the risk of colorectal cancer. Vitamin A supplements should be reserved for undernourished populations and individuals with evidence of vitamin A deficiency.
DEFINITIONS
Lymphomas - a group of blood cancers developing from specific white blood cells called lymphocytes
Neuroblastoma - cancer arising from nerve cells of the central or peripheral nervous system
Tolerable upper intake level (UL) - the highest level of daily intake of a given nutrient that likely poses no risk of adverse effects in almost all individuals of a specific age. The UL for vitamin A in adults is set at 3 mg/day of retinol equivalents (10,000 IU/day).

[Download PDF]

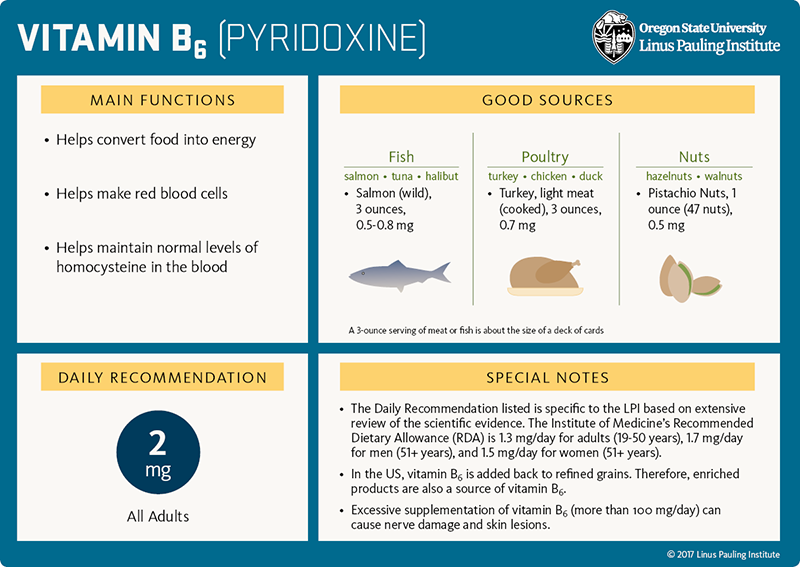
Vitamin B6
What it does
General
-
Vitamin B6 and its derivative pyridoxal 5’-phosphate (PLP) are essential for over 100 enzymes involved in the production of energy and the synthesis of neurotransmitters, hemoglobin, and DNA.
-
Additionally, the B-vitamins folate, vitamin B12, and vitamin B6 work together in the so-called 'one-carbon metabolic pathway' to maintain normal concentrations of homocysteine in blood.
-
Vitamin B6 is found in a variety of foods, including fish, poultry, nuts, legumes, starchy vegetables, avocados, and bananas.
Cancer-specific
-
Deficiency in vitamin B6 may lead to anomalies in DNA synthesis and methylation, thereby contributing to cancer development.
What we know
-
Higher dietary intakes of vitamin B6 and higher blood PLP concentrations are associated with a lower risk of colorectal cancer (29, 38-40).
-
No trial has been designed to examine whether supplementation with vitamin B6 alone could be protective against any cancer, including colorectal cancer (38).
For more information, see the section on Gastrointestinal cancers in the Vitamin B6 article.
[Download PDF]

Vitamin C
What it does
General
-
Vitamin C (ascorbic acid) is a water-soluble vitamin that neutralizes a variety of reactive oxygen species and recycles important cellular antioxidants (including vitamin E).
-
Vitamin C is also a cofactor in enzymatic reactions involved in the regulation of gene expression and in the making of collagen, L-carnitine, and several neurotransmitters.
Cancer-specific
-
Vitamin C is a cofactor for enzymes that influence the methylation of DNA. DNA methylation plays a crucial role in the stability of the genome and alterations of DNA methylation profile are one feature of cancer development.
-
Vitamin C is an antioxidant that might protect the gastrointestinal lining from oxidative damage and contribute to limit the formation of cancer-causing agents like nitrosamines in the stomach (41).
What we know
-
Limited evidence suggests a lower risk of colorectal adenoma (37) — but not colorectal cancer (29, 36, 42) — with higher intakes of vitamin C from food and/or supplements.
DEFINITIONS
Nitrosamines - cancer-causing compounds produced from nitrites and amines derived from proteins either during meat processing or under the strongly acidic condition of the stomach
Oxidative damage - damage caused to large molecules (i.e. carbohydrates, protein, fat, DNA) by the presence of reactive oxygen species
Reactive oxygen species - highly reactive chemicals, containing oxygen, that react easily with other molecules, resulting in potentially damaging modifications

[Download PDF]

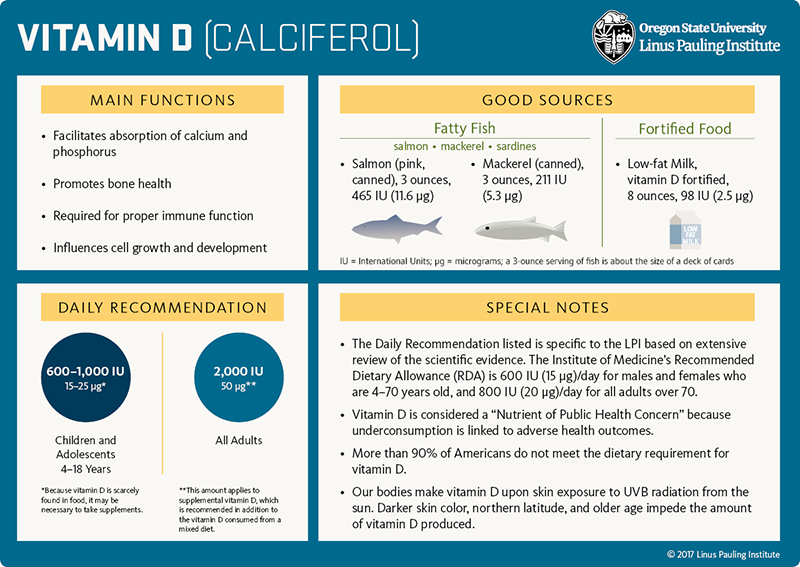
Vitamin D
What it does
General
-
Vitamin D is made in the skin upon sunlight (UV) exposure and can also be obtained from a few foods or supplements.
-
Vitamin D is a fat-soluble vitamin that helps regulate calcium and phosphorus homeostasis, promotes bone health and immune function, and influences cell growth and development.
Cancer-specific
-
Test tube and animal experiments showed that vitamin D can stop the multiplication and trigger the death of various types of cancer cells.
-
Vitamin D helps strengthen the immune system and limit chronic inflammatory processes that often precede cancer development (43).
-
Low vitamin D status has been associated with a higher risk of dying prematurely from cancer.
What we know
-
Adequate vitamin D status is associated with a lower risk of developing colorectal cancer (44, 45) and a better survival rate in patients diagnosed with the disease (46-48).
DEFINITION
Homeostasis - a state of equilibrium in biological systems. Dynamic mechanisms deal with changes in internal and external environments to ensure constancy of physiological conditions.
For more information, see the section on colorectal cancer in the Vitamin D article.
[Download PDF]

Zinc
What it does
General
-
Zinc is an essential trace mineral that is required for the synthesis of hundreds of essential proteins, facilitates oxygen transport and storage, and assists several antioxidant enzymes.
Cancer-specific
-
High intake of red meat, rich in heme iron and zinc, is associated with a higher risk of colorectal cancer.
-
However, unlike iron, zinc is an antioxidant with potential anticancer activities (49, 50).
What we know
-
Dietary zinc deficiency is common, affecting primarily populations in low- and middle-income countries whose diets lack foods of animal origin.
-
Higher zinc intakes from food have been associated with a lower risk of developing colorectal cancer (51, 52).
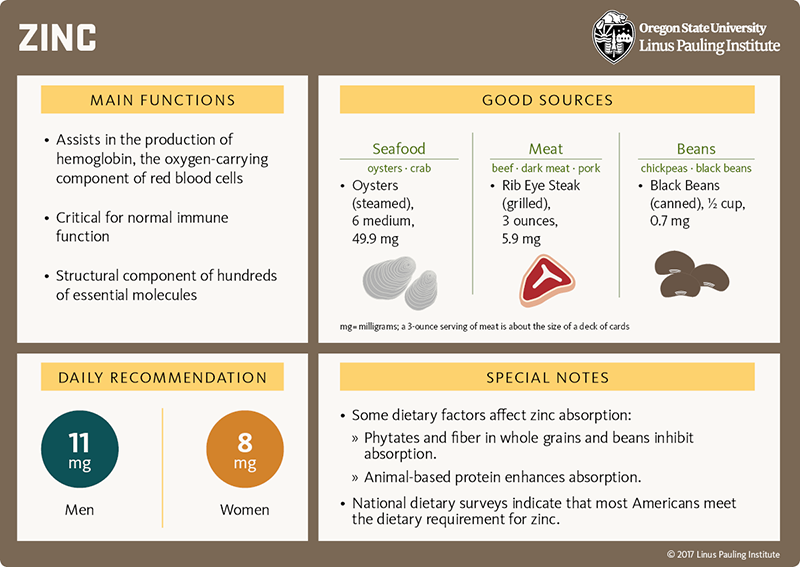
[Download PDF]

HIGHLIGHT
Test tube experiments are performed on isolated cells, grown in a laboratory, that are exposed to high concentrations of a test compound. It is important to keep in mind that test tube and animal experiments provide valuable information but differ from human trials in many ways. The outcome may differ for humans ingesting dietary or supplemental versions of the experimental agent.
Carotenoids
What they do
General
-
Carotenoids are yellow, orange, and red pigments found in fruit and vegetables. We can distinguish:
-
Those which the body can use to form vitamin A; i.e., α-carotene, β-carotene, and β-cryptoxanthin;
-
Those which cannot be converted to vitamin A; i.e., lutein, zeaxanthin, and lycopene.
-
Lutein and zeaxanthin can protect specialized cells in the retina against oxidative damage.
Cancer-specific
-
Carotenoids have demonstrated anticancer activities in test tube experiments (53).
-
Supplementation with β-carotene has not resulted in a reduction in overall cancer risk (54).
-
People at risk for lung cancer, including smokers, are advised not to use β-carotene supplements (54).
What we know
-
Observational studies have found no association between high intakes of carotenoids and the risk of colorectal cancer (55, 56).
-
Regular intake of β-carotene supplements has not been associated with any harm or benefit regarding the risk of colorectal cancer, even in smokers (54).
DEFINITIONS
Anticancer activities - a set of actions that contribute to decreasing the chance for abnormal cells to multiply and spread
Oxidative damage - damage caused to large molecules (i.e., carbohydrates, protein, fat, DNA) by the presence of reactive oxygen species
For references and more information, read the section in the on Carotenoids article.

Curcumin
What it does
General
-
Curcumin is a naturally occurring plant chemical that is abundant in the spice turmeric.
-
Experiments performed in test tubes indicated that curcumin can trigger antioxidant and anti-inflammatory defense systems within cells.
-
Animal experiments showed a protective effect of curcumin against stress-induced ulcers and other lesions of the gastric mucosa caused by the chronic use of drugs (e.g., NSAIDs) (57).
Cancer-specific
-
The results of pilot studies suggest that high doses of oral curcumin might help improve tumor-related markers and provide symptomatic relief in patients with cancer (58).
-
The therapeutic efficacy of oral curcumin administration depends on the bioavailability of curcumin, which is very low since curcumin is readily excreted by the body upon absorption. Innovative solutions are being developed to improve curcumin bioavailability (59).
What we know
-
Oral administration of curcumin (3 g/day for one year) to patients with familial adenomatous polyposis was found to be safe and well tolerated yet had no effect on the size and number of tumors (60).
DEFINITIONS
Bioavailability - the fraction of ingested compound that reaches the circulation and is transported to the site of action
Familial adenomatous polyposis - a hereditary syndrome characterized by the formation of many polyps in the colon and the rectum. Some of the colorectal polyps (adenomas) may become cancerous
NSAIDs - acronym for nonsteroidal anti-inflammatory drugs; NSAIDs reduce pain and inflammation and are prescribed for the symptomatic relief of people affected by chronic inflammatory conditions.
Pilot study - a preliminary study performed to test specific parameters and decide whether a research project could be scaled up.
For references and more information, see the sections on Cancer prevention and Cancer treatment in the article on curcumin.

Flavonoids
What they do
General
-
Flavonoids are plant chemicals that belong to a class of compounds called phenols.
-
Six major subclasses of flavonoids are widely found in edible plants: anthocyanidins, flavan-3-ols, flavonols, flavones, flavanones, and isoflavones.
-
High intakes of flavonoid-rich foods are associated with a 26% lower risk of premature death (61).
Cancer-specific
-
In test tube and animal experiments, flavonoids showed anticancer activities, including abilities to scavenge free radicals, trigger carcinogen excretion, and prevent the multiplication and spread of abnormal cells.
What we know
-
There is no consistent evidence to suggest that high intakes of flavonoid-rich food and beverages are associated with a lower risk of developing colorectal cancer (62-69).
DEFINITIONS
Free radicals - atoms or molecules (with ≥1 unpaired electron) that are highly reactive and can potentially damage large molecules like DNA and lipids; e.g., reactive oxygen species
Carcinogen - cancer-causing agent
For references and more information, see the sections on Cancer prevention and Cancer treatment in the article on flavonoids.

Isothiocyanates
What they do
General
-
Isothiocyanates are compounds formed from glucosinolates found in cruciferous vegetables (e.g., Brussels sprouts, kale, broccoli, bok choy).
-
Most prominent isothiocyanates include benzyl isothiocyanate, phenethyl isothiocyanate, and sulforaphane.
Cancer-specific
-
In animal experiments, isothiocyanates limited the development of chemically induced tumors of several tissues, including the colon.
-
Potential mechanisms of action include the elimination of carcinogens, protection of cells/tissues from oxidative damage, and inhibition of multiplication and spread of cancerous cells.
-
Test tube and animal experiments suggest that isothiocyanates could be beneficial as an adjunct therapy with anticancer drugs (70).
What we know
-
High intakes of cruciferous vegetables may be associated with a lower risk of developing colorectal cancer, yet the available evidence is mixed (71-73).
DEFINITIONS
Adjunct therapy - also called add-on therapy, it refers to a treatment that is given in addition to a standard-of-care protocol in order to enhance efficacy of treatment
Carcinogen - cancer-causing agent
Glucosinolates - sulfur-containing compounds present in cruciferous vegetables. When raw cruciferous vegetables are chopped, glucosinolates are broken down to release isothiocyanates.
Oxidative damage - damage caused to large molecules (i.e., carbohydrates, protein, fat, DNA) by the presence of reactive oxygen species
HIGHLIGHT
Cruciferous vegetables are usually cooked before consumption such that only a small fraction of glucosinolates is broken down to release isothiocyanates. Chop raw cruciferous vegetables, let them sit for several minutes to maximize the formation of isothiocyanates, and steam them for no more than 5 minutes.
For references and more information, see the sections on cancer prevention in the articles on Isothiocyanates and Cruciferous Vegetables.

Phytosterols
What they do
General
-
Phytosterols are compounds that are structurally similar to cholesterol; phytosterols are found in unrefined vegetable oils, whole grains, seeds, nuts, and legumes.
-
Their absorption in our intestine is much lower than that of cholesterol.
-
Phytosterols interfere with intestinal absorption of cholesterol and facilitate the excretion of cholesterol-containing bile in the feces.
-
Daily consumption of phytosterols-enriched foods can lower blood cholesterol concentration.
Cancer-specific
-
Supplementation of animals with phytosterols reduced the multiplication of abnormal cells in chemically induced early lesions and tumors (74).
-
Evidence of a lower risk of cancer with higher intakes of phytosterols in humans is limited to case-control studies (75).
What we know
-
At present, there is not enough evidence to inform whether diets high in phytosterols might reduce the risk of colorectal cancer.

Alcoholic Beverages
What they do
General
-
Alcoholic beverages contain ethanol and other ingredients with bioactive properties and potential health effects.
-
When consumed in moderation (1-2 drinks/day), alcohol consumption has been associated with beneficial effects on the cardiovascular system.
Cancer-specific
-
Even modest intakes of alcohol may increase the risk of cancer (76).
-
Alcohol intake is a risk factor for certain cancers of the digestive system and for breast cancer (76, 77).
What we know
-
Regular intakes of >3 alcoholic drinks/day (>42 g/day) have been associated with a 25% higher risk of colorectal cancer (78). It is unclear whether lower intakes are also associated with a higher risk of colorectal cancer (78, 79).
-
Light alcohol drinking (≤1 drink/day) prior to colorectal cancer diagnosis was associated with lower risks of overall mortality and colorectal cancer-related mortality (when compared to no drinking) (80).
HIGHLIGHT
-
1 standard alcoholic drink contains 14 g of pure alcohol, which is equivalent to:
-
12 fluid ounces (fl oz) of beer (~5% of alcohol);
-
8.5 fl oz of malt liquor (~9% of alcohol);
-
5 fl oz of wine (~12% of alcohol);
-
1.5 fl oz of distilled spirit (liquors; ~40% of alcohol)
-
Alcohol is metabolized differently in women and men such that recommendations have a lower threshold for women
-
No alcohol should be consumed by:
-
Pregnant women or women intending to become pregnant;
-
People taking over-the-counter or prescribed medications with the potential for adverse interactions with alcohol;
-
People planning to drive or engage in activities requiring coordination and alertness;
-
Recovering alcoholics;
-
Anyone aged <21 years (according to US alcohol legislation).
For more information, see the article on Alcoholic Beverages.

Coffee
What it does
General
-
Coffee is a complex mixture of carbohydrates, lipids, amino acids, minerals, and other bioactive compounds like caffeine that can influence human health.
-
Drinking coffee is associated with lower risk developing type 2 diabetes mellitus and a lower risk of dying from cardiovascular disease.
Cancer-specific
-
Some bioactive compounds present in coffee, such as caffeine and a class of phytochemicals called diterpenes, have displayed anticancer activities in experimental studies (81).
-
Lower risks of cancer of the oral cavity, uterus, and liver have been consistently reported in coffee drinkers (81, 82).
-
There is no relationship between coffee consumption and death from cancer overall (82).
What we know
-
Evidence of a reduced risk of colorectal cancer with coffee consumption comes primarily from case-control studies (83-86).
-
Consumption of ≥2 cups of coffee (caffeinated or not) may be associated with better survival rate in people diagnosed with stage I-III colorectal cancer (87).
HIGHLIGHT
Consuming ≤3 cups of filtered coffee daily is unlikely to pose any risk to health in men and in women who are not pregnant. Pregnant women should limit their intake to 1 cup/day, and those breast-feeding should limit coffee intake to 2-3 cups/day.
DEFINITION
Phytochemicals - biologically active molecules found in plants
For more information, see the section on Cancer prevention in the article on coffee.

Dairy Products
What they do
General
-
Dairy products refer to milk and products derived from milk like yogurt, cheese, and butter. Dairy foods are a good source of energy (protein, fat, and carbohydrates), vitamins (e.g., B vitamins, vitamin E, vitamin D [when fortified]), and minerals (e.g., calcium, magnesium, phosphorus, potassium, sodium, zinc) (88).
-
Dairy food consumption plays an important role for bone health across all stages of life by supplying key nutrients (especially calcium, vitamin D, and protein) necessary to build strong bones and limit the occurrence of bone disease and fractures later in life (89).
-
Consumption of dairy products is associated with a lower risk of type 2 diabetes mellitus (90, 91). No such associations have been found with risks of hypertension (92) or cardiovascular disease (93, 94).
HIGHLIGHT
Replacing dairy products with calcium-replacement foods (e.g., bony fish, calcium-set tofu, leafy greens, and fortified beverages [e.g., soy- and almond-based beverages, rice drink, and orange juice]) alter the nutritional profile of one’s diet. For example, substituting soy drinks for low-fat dairy will supply less protein, fat, magnesium, phosphorus, and potassium
(95).
Cancer-specific
-
Dairy products are a major source of conjugated linoleic acid, which has been found to display anticancer activities in experimental studies. The overall nutritional profile of dairy foods may also be important to protect against cancer (88).
-
Some evidence points to higher risks of gastric cancer (96), prostate cancer (97), ovarian cancer (98), and non-Hodgkin lymphoma (99) with higher intakes of milk. However, data are too limited and inconsistent, and no causal relationship has been established (100).
-
There is no evidence of an association between dairy food consumption and the risks of lung (101, 102), pancreatic (103), breast (104, 105), or endometrial (106) cancers.
What we know
-
Higher versus lower intakes of dairy products have been associated with a 20% lower risk of colorectal cancer (107, 108).
-
Consumption of specific dairy products, including total and low-fat milk, yogurt, and cheese, has been associated with a lower risk of colorectal cancer. There is no evidence of an association between consumption of either whole milk or cultured (fermented) milk and risk of colorectal cancer (108).
HIGHLIGHT
Most recommended healthy dietary patterns include the consumption of three servings of dairy foods per day in order to meet the
recommended dietary allowance (RDA) for calcium
(10,
109). The 2015-2020 Dietary Guidelines for Americans recommend to pick fat-free or low-fat dairy alternatives
(10), although be aware that fat may be replaced by sugars in some of these products.
DEFINITIONS
Anticancer activities - a set of actions that contribute to decreasing the chance for abnormal cells to multiply and spread
Recommended Dietary Allowance (RDA) - the average daily dietary intake level of a nutrient sufficient to meet the requirements of nearly all healthy individuals in a specific life stage and gender group
For more information, see the section on colorectal cancer in the Calcium article.

Fish
What they do
General
-
Fish are part of a healthy dietary pattern. They are a good source of protein, long-chain omega-3 fatty acids (a type of polyunsaturated fatty acids), vitamins (B12, D), and essential minerals (iron, zinc, selenium, iodine).
-
High intakes of fish have been associated with lower risks of cardiovascular disease and cognitive deterioration.
Cancer-specific
-
Higher dietary intakes of a number of nutrients provided by fish intake, including omega-3 fatty acids, vitamin D, and zinc, have been associated with lower risks of developing cancer.
-
In animal experiments, oral supplementation with omega-3 fatty acids and their derivatives reduced the risk of cancer by triggering mechanisms against inflammation, oxidative stress, and abnormal cell proliferation (12, 13).
What we know
-
Evidence from prospective cohort studies suggests an 8% lower risk of colorectal cancer with higher versus lower intakes of fish (110).
DEFINITIONS
Cognitive - refers to the processes of cognition, i.e., brain functions like attention, memory, planning, developing strategies, and problem solving
Oxidative stress - a situation in which the production of reactive oxygen species exceeds the ability of an organism to eliminate or neutralize them

Fruit and Vegetables
What they do
General
-
Adherence to diets rich in fruit and vegetables has consistently been associated with lower risks of developing chronic diseases, particularly type 2 diabetes mellitus and cardiovascular disease.
-
Higher intakes of apples, berries, citrus fruit, cruciferous vegetables, and green leafy vegetables have been associated with a lower risk of dying prematurely.
Cancer-specific
-
Daily consumption of five portions (~400 g) of a variety of fruit and non-starchy vegetables is recommended to lower the risk of certain types of cancer (111).
-
Micronutrients (e.g., vitamin C) and phytochemicals (e.g., flavonoids in citrus fruit, organosulfur compounds in garlic and cruciferous vegetables) have anticancer properties likely related to their ability to limit carcinogen formation, activation, and/or toxicity, and to prevent abnormal cell multiplication.
-
Fruit and vegetables are also a great source of dietary fibers that protect the digestive mucosa from exposure to carcinogens and contribute, through their fermentation in the colon, to the formation of short-chain fatty acids with anti-inflammatory and anticancer activities.
What we know
-
There is consistent evidence showing that high intakes of fruit and vegetables are associated with a lower risk of developing colorectal cancer (112-114).
-
Limited evidence from case-control studies suggests that high intakes of cruciferous vegetables may be associated with a lower risk of colorectal cancer (71, 72).
-
There is no evidence of an association between intakes of garlic and risk of colorectal cancer (115, 116).
DEFINITIONS
Carcinogen - a cancer-causing compound
Flavonoids - phenolic compounds widely found in fruit and vegetables; citrus fruit (e.g., oranges, lemons, grapefruit) are rich in a subclass of flavonoids called flavanones
Organosulfur compounds - sulfur-containing molecules. The two main classes of organosulfur compounds found in whole garlic cloves are called L-cysteine sulfoxides and γ-glutamyl-L-cysteine peptides. Organosulfur compounds found in cruciferous vegetables are called isothiocyanates.
Phytochemicals - biologically active molecules found in plants
For references and more information, see the articles on Fruit and Vegetables, Cruciferous Vegetables, and Garlic.

Healthy Diets
What they do
General
-
Healthy dietary plans stress the intake of certain food groups, such as fruit and vegetables, whole grains, nuts and legumes, low-fat dairy products, and lean meat, while playing down the intake of red and processed meats.
-
High intakes of red and processed meats, sugar-sweetened beverages, refined grains, potatoes, and desserts usually characterize unhealthy dietary patterns.
-
Adherence to a healthy dietary pattern, such as the DASH eating plan or the traditional Mediterranean diet, is associated with improved cardiovascular and overall health (117-119).
Cancer-specific
-
High adherence to a Mediterranean-style (120-122) or a DASH-style (123) diet is associated with a lower overall mortality from cancer.
What we know
-
The overall evidence points to a reduced risk of colorectal cancer with higher adherence to diets high in fruit and vegetables and low in meats and sweets. However, this association was mainly apparent in case-control studies and not in prospective cohort studies (124).
-
Pooled analyses of studies indicate that higher adherence to the Mediterranean (122) or DASH diet is associated with an approximately 20% lower risk of colorectal cancer (125).
HIGHLIGHT
The
2015-2020 Dietary Guidelines for Americans provides recommended amounts of foods from each food group corresponding to either a healthy US-style diet (appendix 3), a healthy Mediterranean-style diet (appendix 4), or a healthy vegetarian diet (appendix 6).
DEFINITION
DASH - acronym for dietary approaches to stop hypertension. This balanced eating plan was initially developed to reduce one’s risk of high blood pressure through lowering salt intake.
For more information about the DASH eating plan, visit the National Institutes of Health website.

Legumes
What they do
General
-
Foods from the legume family include beans, peas, lentils, soybeans, and peanuts.
-
Legumes are a good source of protein, essential minerals (magnesium, potassium, iron, zinc), vitamins (folate), fiber, and phytochemicals (flavonoids and phytosterols).
Cancer-specific
-
Soybeans are a good source of isoflavones, which are structurally similar to mammalian estrogens. The anti-estrogenic properties of isoflavones may be useful to prevent hormonally driven cancers like cancers of the breast and prostate.
-
Legumes are a good source of fiber; higher fiber intake is beneficial to gastrointestinal health and may help prevent cancers of the gastrointestinal tract.
What we know
-
There is no consistent evidence to suggest a lower risk of colorectal cancer with higher intakes of legumes, legume fibers, soy products, or isoflavones (66, 113, 114, 126-128) .
For more information, see the section on cancer prevention in the Legumes article.

Nuts
What they do
General
-
Nuts are a good source of soluble fiber, phytosterols, polyphenols, mono- and polyunsaturated fatty acids, protein, and certain vitamins (folate, vitamin E) and minerals (calcium, magnesium, potassium).
-
Examples of tree nuts include almonds, Brazil nuts, cashews, hazelnuts, macadamia nuts, pecans, pistachios, and walnuts.
-
Peanuts are not nuts; they are legumes. However, peanuts are nutritionally similar to tree nuts and offer some of the same health benefits.
-
Regular nut consumption (1 ounce at least 5 times per week) is associated with a significantly lower risk of developing or dying from coronary heart disease.
Cancer-specific
-
Several nutritional components present in nuts and peanuts — fiber (129), phytochemicals (130-134), micronutrients (135), and mono/polyunsaturated fatty acids (136) — may protect against cancer.
-
Nut consumption has been inversely associated with the risk of specific cancer types, including ovarian cancer (137), prostate cancer (137), and non-cardia gastric cancer (138, 139).
-
Nut consumption is also associated with a lower risk of premature death by cancer (140).
What we know
-
There is little evidence to suggest a lower risk of colorectal cancer with tree nut and peanut consumption (113, 137).
-
One prospective cohort study in people who had a stage III colorectal tumor found that higher (vs. lower) nut intake was associated with less risk of tumor recurrence and better survival over a six-year period (141).
HIGHLIGHT
-
Nuts are packed with healthy fats, and therefore, calories.
-
1 ounce of nuts contains approximately 160 kcal and 14-19 g of fat (mainly mono- and polyunsaturated fatty acids)
-
1 ounce of nuts equals approximately: 24 almonds, 8 medium Brazil nuts*, 18 medium cashews, 12 hazelnuts, 12 macadamia nuts, 15 pecan halves, 47 pistachios, 14 walnut halves, and 35 peanuts.
-
It is recommended to substitute nuts for sources of saturated fat and junk food.
*Depending on growth conditions, a single Brazil nut could contain an extremely high amount of selenium.
DEFINITIONS
Inverse association - a relationship between two variables in which they move in opposite directions
Phytochemicals - biologically active molecules found in plants
Tumor recurrence - refers to a tumor that comes back in the same place or close by, after a period of time during which it could not be detected
For more information, see the section on cancer prevention in the Nuts article.

Red and Processed Meats
What they do
General
-
Meat is a good source of protein, vitamins (vitamin A and B vitamins), and minerals (iron, zinc, selenium, phosphorus). The fat content of meat varies across retail cuts of beef, poultry, and other meats, as well as with processing techniques and cooking methods (142).
-
Red meat refers to meat of beef, veal, pork, lamb, sheep, horse, and goat. Processed meat usually refers to products made of red meat that are cured, salted, or smoked and contain high amounts of minced fatty tissues (e.g., sausages) (143). Thus, processed meats usually have a higher content of saturated fat, cholesterol, salt (sodium chloride), and nitrates than fresh, unprocessed red meats (144).
-
Long-term consumption of red meat, especially if processed, has been associated with higher risks of type 2 diabetes mellitus, cardiovascular disease, and premature death (144).
Cancer-specific
-
Several molecules generated during meat processing (e.g., N-nitroso-compounds, polycyclic aromatic hydrocarbons) or when meat is heated at high temperatures (e.g., heterocyclic aromatic amines) are suspected or well-known carcinogens. Other mechanisms involving, for example, the oncogenic effect of heme iron (much more abundant in red than white meat) have been suggested to explain the potential hazards associated with consuming red and processed meat (144).
-
Limited evidence suggests that consuming large amounts of red and/or processed meat is associated with higher risks of esophageal, stomach, liver, and bladder cancer (143, 144).
What we know
-
High consumption of processed meat is associated with a high risk of colorectal cancer (113, 114, 145).
-
Recent pooled analyses also suggest that high intake of red meat is a risk factor for colorectal cancer (113, 114). Limited evidence indicates that high intakes of beef and lamb, but not pork and poultry, are associated with a higher risk of colorectal cancer (146).
HIGHLIGHT
Reducing the consumption of red and processed meat in high-consuming countries is generally recommended for both environmental and health concerns. Guidelines from the American Cancer Society suggest to reduce red and processed meat consumption by (9):
-
Limiting the consumption of bacon, sausage, luncheon meats, and hot dogs
-
Choosing fish, poultry, or beans as an alternative to red meat
-
Opting for lean cuts and eating smaller portions of red meat
-
Preparing meat, poultry, and fish by baking, broiling, or poaching rather than frying or charbroiling
DEFINITION
Carcinogen - cancer-causing agent
Oncogenic effect - ability to cause the development of a tumor

Tea
What it does
General
-
Tea is an infusion of the leaves of the Camellia sinensis plant and includes white, green, oolong, and black teas. This summary does not discuss herbal teas, which are infusions of herbs or plants other than Camellia sinensis.
-
Tea contains a number of bioactive substances, including caffeine, fluoride, and flavonoids (primarily flavan-3-ols), which may exert health effects. Daily consumption of 2-4 cups of tea is associated with lower risks of type 2 diabetes and cardiovascular disease (147).
Cancer-specific
-
Tea is particularly rich in catechins (flavan-3-ol monomers), a subclass of flavonoids with antioxidant properties that could protect in particular the epithelium of the digestive tract against oxidative injury, block the activation of carcinogen, and interfere with cancer cell multiplication (148).
-
Tea consumption has not been associated with lower risks of any cancer types except cancers of the oral cavity (149).
What we know
-
There is no consistent evidence to suggest that higher intakes of tea are associated with a reduced risk of developing colorectal cancer (114, 150, 151).
HIGHLIGHT
Consuming very hot beverages (including very hot tea, i.e.,
>65°C or >149°F) may damage the cells lining the upper digestive tract and specifically increase the risk of esophageal
(152) and stomach
(153) cancers.
For more information, see the section on cancer prevention in the Tea article.

Whole Grains
What they do
General
-
Whole grains are the seeds of plants belonging to the grass family. The grass family includes wheat, rice, maize (corn), barley, oats, and rye.
-
Whole-grain products contain all three layers of the seed: bran, endosperm, and germ.
-
In contrast to whole grains, refined grains are stripped of the bran and germ layers. Some essential micronutrients (thiamin, riboflavin, niacin, iron) are sometimes added back to the grain after the refining process, producing what is known as an "enriched grain."
Cancer-specific
-
Whole grains contain several nutrients and dietary factors that are associated with cancer risk reduction.
-
The fermentation of dietary fiber in the large intestine produces short-chain fatty acids with anticancer properties. Fiber also protects the digestive tract by diluting carcinogens in the fecal bulk and speeding up transit (154).
-
Antioxidants (e.g., polyphenols, carotenoids, ferulic acid, vitamin E, and minerals like iron, zinc, copper, and selenium) protect tissues against oxidative damage that increases the risk of cancer (154).
-
Consumption of fiber-rich whole grains improves glucose and lipid metabolism. Metabolic disorders like obesity and diabetes are risk factors for colorectal cancer (155).
-
High intakes of whole grains have been associated with a lower risk of death by cancer (156-158).
What we know
-
Consuming about three servings (90 g) of whole-grain products per day is associated with a nearly 20% lower risk of colorectal cancer (114, 126).
HIGHLIGHT
The 2015-2020 Dietary Guidelines for Americans recommend consuming a minimum of three servings of whole-grain products daily.
Examples of one serving of whole grains:
-
1 slice of whole-grain bread
-
½ whole-grain English muffin, bagel, or bun
-
1 ounce of ready-to-eat whole-grain cereal
-
½ cup of oatmeal, brown rice, or whole-wheat pasta (cooked)
-
5-6 whole-grain crackers
-
1 tortilla (6” diameter)
-
1 pancake (5” diameter)
DEFINITIONS
Carcinogen - cancer-causing agent
Oxidative damage - damage caused to large molecules (i.e., carbohydrates, protein, fat, DNA) by the presence of reactive oxygen species
For general information, see the Whole Grains article.

References
1. International Agency for Research on Cancer. Global Cancer Observatory: Colorectal cancer fact sheet. Available at: http://gco.iarc.fr/today/data/factsheets/cancers/10_8_9-Colorectum-fact-sheet.pdf. Accessed 7/19/19.
2. Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global patterns and trends in colorectal cancer incidence and mortality. Gut. 2017;66(4):683-691. (PubMed)
3. Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/cancer/colorectal/index.htm.
4. Vogelstein B, Fearon ER, Hamilton SR, et al. Genetic alterations during colorectal-tumor development. N Engl J Med. 1988;319(9):525-532. (PubMed)
5. Aran V, Victorino AP, Thuler LC, Ferreira CG. Colorectal cancer: epidemiology, disease mechanisms and interventions to reduce onset and mortality. Clin Colorectal Cancer. 2016;15(3):195-203. (PubMed)
6. Phipps AI, Limburg PJ, Baron JA, et al. Association between molecular subtypes of colorectal cancer and patient survival. Gastroenterology. 2015;148(1):77-87.e72. (PubMed)
7. Kuipers EJ, Grady WM, Lieberman D, et al. Colorectal cancer. Nat Rev Dis Primers. 2015;1:15065. (PubMed)
8. Connell LC, Mota JM, Braghiroli MI, Hoff PM. The rising incidence of younger patients with colorectal cancer: questions about screening, biology, and treatment. Curr Treat Options Oncol. 2017;18(4):23. (PubMed)
9. Kushi LH, Doyle C, McCullough M, et al. American Cancer Society Guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin. 2012;62(1):30-67. (PubMed)
10. US Department of Health and Human Services and US Department of Agriculture. 2015-2020 Dietary Guidelines for Americans. Available at: https://health.gov/dietaryguidelines/2015/guidelines/. Accessed 7/22/19.
11. Imamura F, Micha R, Wu JH, et al. Effects of saturated fat, polyunsaturated fat, monounsaturated fat, and carbohydrate on glucose-insulin homeostasis: a systematic review and meta-analysis of randomised controlled feeding trials. PLoS Med. 2016;13(7):e1002087. (PubMed)
12. Lee HJ, Han YM, An JM, et al. Role of omega-3 polyunsaturated fatty acids in preventing gastrointestinal cancers: current status and future perspectives. Expert Rev Anticancer Ther. 2018;18(12):1189-1203. (PubMed)
13. Volpato M, Hull MA. Omega-3 polyunsaturated fatty acids as adjuvant therapy of colorectal cancer. Cancer Metastasis Rev. 2018;37(2-3):545-555. (PubMed)
14. Kim M, Park K. Dietary fat intake and risk of colorectal cancer: a systematic review and meta-analysis of prospective studies. Nutrients. 2018;10(12). (PubMed)
15. McRae MP. The benefits of dietary fiber intake on reducing the risk of cancer: an umbrella review of meta-analyses. J Chiropr Med. 2018;17(2):90-96. (PubMed)
16. Iamartino L, Elajnaf T, Kallay E, Schepelmann M. Calcium-sensing receptor in colorectal inflammation and cancer: Current insights and future perspectives. World J Gastroenterol. 2018;24(36):4119-4131. (PubMed)
17. Meng Y, Sun J, Yu J, Wang C, Su J. Dietary intakes of calcium, iron, magnesium, and potassium elements and the risk of colorectal cancer: a meta-analysis. Biol Trace Elem Res. 2019;189(2):325-335. (PubMed)
18. Keum N, Giovannucci EL. Folic acid fortification and colorectal cancer risk. Am J Prev Med. 2014;46(3 Suppl 1):S65-72. (PubMed)
19. Bonovas S, Fiorino G, Lytras T, Malesci A, Danese S. Calcium supplementation for the prevention of colorectal adenomas: A systematic review and meta-analysis of randomized controlled trials. World J Gastroenterol. 2016;22(18):4594-4603. (PubMed)
20. Veettil SK, Ching SM, Lim KG, Saokaew S, Phisalprapa P, Chaiyakunapruk N. Effects of calcium on the incidence of recurrent colorectal adenomas: A systematic review with meta-analysis and trial sequential analysis of randomized controlled trials. Medicine (Baltimore). 2017;96(32):e7661. (PubMed)
21. Moazzen S, Dolatkhah R, Tabrizi JS, et al. Folic acid intake and folate status and colorectal cancer risk: A systematic review and meta-analysis. Clin Nutr. 2018;37(6 Pt A):1926-1934. (PubMed)
22. Jennings BA, Willis G. How folate metabolism affects colorectal cancer development and treatment; a story of heterogeneity and pleiotropy. Cancer Lett. 2015;356(2 Pt A):224-230. (PubMed)
23. Burr NE, Hull MA, Subramanian V. Folic acid supplementation may reduce colorectal cancer risk in patients with inflammatory bowel disease: a systematic review and meta-analysis. J Clin Gastroenterol. 2017;51(3):247-253. (PubMed)
24. Mason JB, Tang SY. Folate status and colorectal cancer risk: A 2016 update. Mol Aspects Med. 2017;53:73-79. (PubMed)
25. Qin T, Du M, Du H, Shu Y, Wang M, Zhu L. Folic acid supplements and colorectal cancer risk: meta-analysis of randomized controlled trials. Sci Rep. 2015;5:12044. (PubMed)
26. Passarelli MN, Barry EL, Rees JR, et al. Folic acid supplementation and risk of colorectal neoplasia during long-term follow-up of a randomized clinical trial. Am J Clin Nutr. 2019; 110(4):903-911. (PubMed)
27. Food Fortification Initiatives. Global progress of industrially milled cereal grain fortification. August 2019. http://www.ffinetwork.org/global_progress/. Accessed 8/10/19.
28. Fonseca-Nunes A, Jakszyn P, Agudo A. Iron and cancer risk--a systematic review and meta-analysis of the epidemiological evidence. Cancer Epidemiol Biomarkers Prev. 2014;23(1):12-31. (PubMed)
29. Liu Y, Yu Q, Zhu Z, et al. Vitamin and multiple-vitamin supplement intake and incidence of colorectal cancer: a meta-analysis of cohort studies. Med Oncol. 2015;32(1):434. (PubMed)
30. Liu Y, Yu QY, Zhu ZL, Tang PY, Li K. Vitamin B2 intake and the risk of colorectal cancer: a meta-analysis of observational studies. Asian Pac J Cancer Prev. 2015;16(3):909-913. (PubMed)
31. Yoon YS, Jung S, Zhang X, Ogino S, Giovannucci EL, Cho E. Vitamin B2 intake and colorectal cancer risk; results from the Nurses' Health Study and the Health Professionals Follow-Up Study cohort. Int J Cancer. 2016;139(5):996-1008. (PubMed)
32. Vinceti M, Filippini T, Del Giovane C, et al. Selenium for preventing cancer. Cochrane Database Syst Rev. 2018;1:Cd005195. (PubMed)
33. Cai X, Wang C, Yu W, et al. Selenium exposure and cancer risk: an updated meta-analysis and meta-regression. Sci Rep. 2016;6:19213. (PubMed)
34. Bouriez D, Giraud J, Gronnier C, Varon C. Efficiency of all-trans tetinoic acid on gastric cancer: a narrative literature review. Int J Mol Sci. 2018;19(11). (PubMed)
35. Dobrotkova V, Chlapek P, Mazanek P, Sterba J, Veselska R. Traffic lights for retinoids in oncology: molecular markers of retinoid resistance and sensitivity and their use in the management of cancer differentiation therapy. BMC Cancer. 2018;18(1):1059. (PubMed)
36. Heine-Broring RC, Winkels RM, Renkema JM, et al. Dietary supplement use and colorectal cancer risk: a systematic review and meta-analyses of prospective cohort studies. Int J Cancer. 2015;136(10):2388-2401. (PubMed)
37. Xu X, Yu E, Liu L, et al. Dietary intake of vitamins A, C, and E and the risk of colorectal adenoma: a meta-analysis of observational studies. Eur J Cancer Prev. 2013;22(6):529-539. (PubMed)
38. Mocellin S, Briarava M, Pilati P. Vitamin B6 and cancer risk: a field synopsis and meta-analysis. J Natl Cancer Inst. 2017;109(3):1-9. (PubMed)
39. Jia K, Wang R, Tian J. Vitamin B6 intake and the risk of colorectal cancer: a meta-analysis of prospective cohort studies. Nutr Cancer. 2017;69(5):723-731. (PubMed)
40. Larsson SC, Orsini N, Wolk A. Vitamin B6 and risk of colorectal cancer: a meta-analysis of prospective studies. JAMA. 2010;303(11):1077-1083. (PubMed)
41. Vingeliene S, Chan DS, Aune D, et al. An update of the WCRF/AICR systematic literature review on esophageal and gastric cancers and citrus fruits intake. Cancer Causes Control. 2016;27(7):837-851. (PubMed)
42. Park Y, Spiegelman D, Hunter DJ, et al. Intakes of vitamins A, C, and E and use of multiple vitamin supplements and risk of colon cancer: a pooled analysis of prospective cohort studies. Cancer Causes Control. 2010;21(11):1745-1757. (PubMed)
43. Meeker S, Seamons A, Maggio-Price L, Paik J. Protective links between vitamin D, inflammatory bowel disease and colon cancer. World J Gastroenterol. 2016;22(3):933-948. (PubMed)
44. Ekmekcioglu C, Haluza D, Kundi M. 25-Hydroxyvitamin D status and risk for colorectal cancer and type 2 diabetes mellitus: a systematic review and meta-analysis of epidemiological studies. Int J Environ Res Public Health. 2017;14(2). (PubMed)
45. Garland CF, Gorham ED. Dose-response of serum 25-hydroxyvitamin D in association with risk of colorectal cancer: A meta-analysis. J Steroid Biochem Mol Biol. 2017;168:1-8. (PubMed)
46. Hamada T, Liu L, Nowak JA, et al. Vitamin D status after colorectal cancer diagnosis and patient survival according to immune response to tumour. Eur J Cancer. 2018;103:98-107. (PubMed)
47. Maalmi H, Walter V, Jansen L, et al. Association between blood 25-hydroxyvitamin D levels and survival in colorectal cancer patients: an updated systematic review and meta-analysis. Nutrients. 2018;10(7). (PubMed)
48. Ng K, Nimeiri HS, McCleary NJ, et al. Effect of high-dose vs standard-dose vitamin D3 supplementation on progression-free survival among patients with advanced or metastatic colorectal cancer: The SUNSHINE randomized clinical trial. JAMA. 2019;321(14):1370-1379. (PubMed)
49. Prasad AS. Clinical, immunological, anti-inflammatory and antioxidant roles of zinc. Exp Gerontol. 2008;43(5):370-377. (PubMed)
50. Prasad AS, Beck FW, Snell DC, Kucuk O. Zinc in cancer prevention. Nutr Cancer. 2009;61(6):879-887. (PubMed)
51. Li P, Xu J, Shi Y, et al. Association between zinc intake and risk of digestive tract cancers: a systematic review and meta-analysis. Clin Nutr. 2014;33(3):415-420. (PubMed)
52. Qiao L, Feng Y. Intakes of heme iron and zinc and colorectal cancer incidence: a meta-analysis of prospective studies. Cancer Causes Control. 2013;24(6):1175-1183. (PubMed)
53. Milani A, Basirnejad M, Shahbazi S, Bolhassani A. Carotenoids: biochemistry, pharmacology and treatment. Br J Pharmacol. 2017;174(11):1290-1324. (PubMed)
54. Druesne-Pecollo N, Latino-Martel P, Norat T, et al. Beta-carotene supplementation and cancer risk: a systematic review and meta-analysis of randomized controlled trials. Int J Cancer. 2010;127(1):172-184. (PubMed)
55. Panic N, Nedovic D, Pastorino R, Boccia S, Leoncini E. Carotenoid intake from natural sources and colorectal cancer: a systematic review and meta-analysis of epidemiological studies. Eur J Cancer Prev. 2017;26(1):27-37. (PubMed)
56. Wang X, Yang HH, Liu Y, Zhou Q, Chen ZH. Lycopene consumption and risk of colorectal cancer: a meta-analysis of observational studies. Nutr Cancer. 2016;68(7):1083-1096. (PubMed)
57. Kwiecien S, Magierowski M, Majka J, et al. Curcumin: a potent protectant against esophageal and gastric disorders. Int J Mol Sci. 2019;20(6). (PubMed)
58. Salehi B, Stojanovic-Radic Z, Matejic J, et al. The therapeutic potential of curcumin: A review of clinical trials. Eur J Med Chem. 2019;163:527-545. (PubMed)
59. Kerdsakundee N, Mahattanadul S, Wiwattanapatapee R. Development and evaluation of gastroretentive raft forming systems incorporating curcumin-Eudragit(R) EPO solid dispersions for gastric ulcer treatment. Eur J Pharm Biopharm. 2015;94:513-520. (PubMed)
60. Cruz-Correa M, Hylind LM, Marrero JH, et al. Efficacy and safety of curcumin in treatment of intestinal adenomas in patients with familial adenomatous polyposis. Gastroenterology. 2018;155(3):668-673. (PubMed)
61. Grosso G, Micek A, Godos J, et al. Dietary flavonoid and lignan intake and mortality in prospective cohort studies: systematic review and dose-response meta-analysis. Am J Epidemiol. 2017;185(12):1304-1316. (PubMed)
62. Bo Y, Sun J, Wang M, Ding J, Lu Q, Yuan L. Dietary flavonoid intake and the risk of digestive tract cancers: a systematic review and meta-analysis. Sci Rep. 2016;6:24836. (PubMed)
63. Chang H, Lei L, Zhou Y, Ye F, Zhao G. Dietary flavonoids and the risk of colorectal cancer: an updated meta-analysis of epidemiological studies. Nutrients. 2018;10(7). (PubMed)
64. He X, Sun LM. Dietary intake of flavonoid subclasses and risk of colorectal cancer: evidence from population studies. Oncotarget. 2016;7(18):26617-26627. (PubMed)
65. Jiang R, Botma A, Rudolph A, Husing A, Chang-Claude J. Phyto-oestrogens and colorectal cancer risk: a systematic review and dose-response meta-analysis of observational studies. Br J Nutr. 2016;116(12):2115-2128. (PubMed)
66. Tse G, Eslick GD. Soy and isoflavone consumption and risk of gastrointestinal cancer: a systematic review and meta-analysis. Eur J Nutr. 2016;55(1):63-73. (PubMed)
67. Wang X, Yang DY, Yang LQ, Zhao WZ, Cai LY, Shi HP. Anthocyanin consumption and risk of colorectal cancer: a meta-analysis of observational studies. J Am Coll Nutr. 2019;38(5):470-477. (PubMed)
68. Woo HD, Kim J. Dietary flavonoid intake and risk of stomach and colorectal cancer. World J Gastroenterol. 2013;19(7):1011-1019. (PubMed)
69. Yu Y, Jing X, Li H, Zhao X, Wang D. Soy isoflavone consumption and colorectal cancer risk: a systematic review and meta-analysis. Sci Rep. 2016;6:25939. (PubMed)
70. Minarini A, Milelli A, Fimognari C, Simoni E, Turrini E, Tumiatti V. Exploring the effects of isothiocyanates on chemotherapeutic drugs. Expert Opin Drug Metab Toxicol. 2014;10(1):25-38. (PubMed)
71. Tse G, Eslick GD. Cruciferous vegetables and risk of colorectal neoplasms: a systematic review and meta-analysis. Nutr Cancer. 2014;66(1):128-139. (PubMed)
72. Wu QJ, Yang Y, Vogtmann E, et al. Cruciferous vegetables intake and the risk of colorectal cancer: a meta-analysis of observational studies. Ann Oncol. 2013;24(4):1079-1087. (PubMed)
73. Johnson IT. Cruciferous vegetables and risk of cancers of the gastrointestinal tract. Mol Nutr Food Res. 2018;62(18):e1701000. (PubMed)
74. Shahzad N, Khan W, Md S, et al. Phytosterols as a natural anticancer agent: Current status and future perspective. Biomed Pharmacother. 2017;88:786-794. (PubMed)
75. Jiang L, Zhao X, Xu J, et al. The protective effect of dietary phytosterols on cancer risk: a systematic meta-analysis. J Oncol. 2019;2019:7479518. (PubMed)
76. LoConte NK, Brewster AM, Kaur JS, Merrill JK, Alberg AJ. Alcohol and cancer: a statement of the American Society of Clinical Oncology. J Clin Oncol. 2018;36(1):83-93. (PubMed)
77. Van't Veer P, Kampman E. Food, Nutrition, Physical Activity, and the Prevention of Cancer: a global perspective. 2007.
78. McNabb S, Harrison TA, Albanes D, et al. Meta-analysis of 16 studies of the association of alcohol with colorectal cancer. Int J Cancer. 2019;146(3):861-873. (PubMed)
79. Choi YJ, Myung SK, Lee JH. Light alcohol drinking and risk of cancer: a meta-analysis of cohort studies. Cancer Res Treat. 2018;50(2):474-487. (PubMed)
80. Kim Y, Je Y, Giovannucci EL. Association between alcohol consumption and survival in colorectal cancer: A meta-analysis. Cancer Epidemiol Biomarkers Prev. 2019;28(11):1891-1901. (PubMed)
81. Bohn SK, Blomhoff R, Paur I. Coffee and cancer risk, epidemiological evidence, and molecular mechanisms. Mol Nutr Food Res. 2014;58(5):915-930. (PubMed)
82. Alicandro G, Tavani A, La Vecchia C. Coffee and cancer risk: a summary overview. Eur J Cancer Prev. 2017;26(5):424-432. (PubMed)
83. Akter S, Kashino I, Mizoue T, et al. Coffee drinking and colorectal cancer risk: an evaluation based on a systematic review and meta-analysis among the Japanese population. Jpn J Clin Oncol. 2016;46(8):781-787. (PubMed)
84. Gan Y, Wu J, Zhang S, et al. Association of coffee consumption with risk of colorectal cancer: a meta-analysis of prospective cohort studies. Oncotarget. 2017;8(12):18699-18711. (PubMed)
85. Li G, Ma D, Zhang Y, Zheng W, Wang P. Coffee consumption and risk of colorectal cancer: a meta-analysis of observational studies. Public Health Nutr. 2013;16(2):346-357. (PubMed)
86. Wang Y, Chen J, Zhao R, et al. Dose-response meta-analysis of coffee consumption and risk of colorectal adenoma. Eur J Clin Nutr. 2019 [Epub ahead of print]. (PubMed)
87. Hu Y, Ding M, Yuan C, et al. Association between coffee intake after diagnosis of colorectal cancer and reduced mortality. Gastroenterology. 2018;154(4):916-926.e919. (PubMed)
88. Tunick MH, Van Hekken DL. Dairy products and health: recent insights. J Agric Food Chem. 2015;63(43):9381-9388. (PubMed)
89. Rozenberg S, Body JJ, Bruyere O, et al. Effects of dairy products consumption on health: benefits and beliefs--a commentary from the Belgian Bone Club and the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases. Calcif Tissue Int. 2016;98(1):1-17. (PubMed)
90. Gijsbers L, Ding EL, Malik VS, de Goede J, Geleijnse JM, Soedamah-Muthu SS. Consumption of dairy foods and diabetes incidence: a dose-response meta-analysis of observational studies. Am J Clin Nutr. 2016;103(4):1111-1124. (PubMed)
91. Schwingshackl L, Hoffmann G, Lampousi AM, et al. Food groups and risk of type 2 diabetes mellitus: a systematic review and meta-analysis of prospective studies. Eur J Epidemiol. 2017;32(5):363-375. (PubMed)
92. Ding M, Huang T, Bergholdt HK, Nordestgaard BG, Ellervik C, Qi L. Dairy consumption, systolic blood pressure, and risk of hypertension: Mendelian randomization study. BMJ. 2017;356:j1000. (PubMed)
93. Guo J, Astrup A, Lovegrove JA, Gijsbers L, Givens DI, Soedamah-Muthu SS. Milk and dairy consumption and risk of cardiovascular diseases and all-cause mortality: dose-response meta-analysis of prospective cohort studies. Eur J Epidemiol. 2017;32(4):269-287. (PubMed)
94. Liang J, Zhou Q, Kwame Amakye W, Su Y, Zhang Z. Biomarkers of dairy fat intake and risk of cardiovascular disease: A systematic review and meta analysis of prospective studies. Crit Rev Food Sci Nutr. 2018;58(7):1122-1130. (PubMed)
95. Fulgoni VL, 3rd, Keast DR, Auestad N, Quann EE. Nutrients from dairy foods are difficult to replace in diets of Americans: food pattern modeling and an analyses of the National Health and Nutrition Examination Survey 2003-2006. Nutr Res. 2011;31(10):759-765. (PubMed)
96. Wang S, Zhou M, Ji A, Zhang D, He J. Milk/dairy products consumption and gastric cancer: an update meta-analysis of epidemiological studies. Oncotarget. 2018;9(6):7126-7135. (PubMed)
97. Lopez-Plaza B, Bermejo LM, Santurino C, Cavero-Redondo I, Alvarez-Bueno C, Gomez-Candela C. Milk and dairy product consumption and prostate cancer risk and mortality: an overview of systematic reviews and meta-analyses. Adv Nutr. 2019;10(suppl_2):S212-s223. (PubMed)
98. Liu J, Tang W, Sang L, et al. Milk, yogurt, and lactose intake and ovarian cancer risk: a meta-analysis. Nutr Cancer. 2015;67(1):68-72. (PubMed)
99. Wang J, Li X, Zhang D. Dairy product consumption and risk of non-Hodgkin lymphoma: a meta-analysis. Nutrients. 2016;8(3):120. (PubMed)
100. Thorning TK, Raben A, Tholstrup T, Soedamah-Muthu SS, Givens I, Astrup A. Milk and dairy products: good or bad for human health? An assessment of the totality of scientific evidence. Food Nutr Res. 2016;60:32527. (PubMed)
101. Yang Y, Wang X, Yao Q, Qin L, Xu C. Dairy product, calcium intake and lung cancer risk: a systematic review with meta-analysis. Sci Rep. 2016;6:20624. (PubMed)
102. Yu Y, Li H, Xu K, et al. Dairy consumption and lung cancer risk: a meta-analysis of prospective cohort studies. Onco Targets Ther. 2016;9:111-116. (PubMed)
103. Genkinger JM, Wang M, Li R, et al. Dairy products and pancreatic cancer risk: a pooled analysis of 14 cohort studies. Ann Oncol. 2014;25(6):1106-1115. (PubMed)
104. Chen L, Li M, Li H. Milk and yogurt intake and breast cancer risk: A meta-analysis. Medicine (Baltimore). 2019;98(12):e14900. (PubMed)
105. Zang J, Shen M, Du S, Chen T, Zou S. The association between dairy intake and breast cancer in Western and Asian populations: a systematic review and meta-analysis. J Breast Cancer. 2015;18(4):313-322. (PubMed)
106. Li X, Zhao J, Li P, Gao Y. Dairy products intake and endometrial cancer risk: a meta-analysis of observational studies. Nutrients. 2017;10(1). (PubMed)
107. Aune D, Lau R, Chan DS, et al. Dairy products and colorectal cancer risk: a systematic review and meta-analysis of cohort studies. Ann Oncol. 2012;23(1):37-45. (PubMed)
108. Barrubes L, Babio N, Becerra-Tomas N, Rosique-Esteban N, Salas-Salvado J. Association between dairy product consumption and colorectal cancer risk in adults: a systematic review and meta-analysis of epidemiologic studies. Adv Nutr. 2019;10(suppl_2):S190-s211. (PubMed)
109. US Department of Agriculture. MyPlate. Available at: https://www.choosemyplate.gov/.
110. Zhang CJ, Chen PF. High consumption of fish tends to be inversely associated with the risk of colorectal cancer. Clin Gastroenterol Hepatol. 2019 [Epub ahead of print]. (PubMed)
111. World Cancer Research Fund/American Institute for Cancer Research. Food, nutrition, physical activity, and the prevention of cancer: a global perspective: Amer Inst for Cancer Research; 2007.
112. Aune D, Lau R, Chan DS, et al. Nonlinear reduction in risk for colorectal cancer by fruit and vegetable intake based on meta-analysis of prospective studies. Gastroenterology. 2011;141(1):106-118. (PubMed)
113. Schwingshackl L, Schwedhelm C, Hoffmann G, et al. Food groups and risk of colorectal cancer. Int J Cancer. 2018;142(9):1748-1758. (PubMed)
114. Vieira AR, Abar L, Chan DSM, et al. Foods and beverages and colorectal cancer risk: a systematic review and meta-analysis of cohort studies, an update of the evidence of the WCRF-AICR Continuous Update Project. Ann Oncol. 2017;28(8):1788-1802. (PubMed)
115. Chiavarini M, Minelli L, Fabiani R. Garlic consumption and colorectal cancer risk in man: a systematic review and meta-analysis. Public Health Nutr. 2016;19(2):308-317. (PubMed)
116. Zhu B, Zou L, Qi L, Zhong R, Miao X. Allium vegetables and garlic supplements do not reduce risk of colorectal cancer, based on meta-analysis of prospective studies. Clin Gastroenterol Hepatol. 2014;12(12):1991-2001.e1991-1994; quiz e1121. (PubMed)
117. Chiavaroli L, Viguiliouk E, Nishi SK, et al. DASH dietary pattern and cardiometabolic outcomes: an umbrella review of systematic reviews and meta-analyses. Nutrients. 2019;11(2). (PubMed)
118. Schwingshackl L, Bogensberger B, Hoffmann G. Diet quality as assessed by the healthy eating index, alternate healthy eating index, Dietary Approaches to Stop Hypertension score, and health outcomes: an updated systematic review and meta-analysis of cohort studies. J Acad Nutr Diet. 2018;118(1):74-100.e111. (PubMed)
119. Sofi F, Macchi C, Abbate R, Gensini GF, Casini A. Mediterranean diet and health status: an updated meta-analysis and a proposal for a literature-based adherence score. Public Health Nutr. 2014;17(12):2769-2782. (PubMed)
120. Del Bo C, Marino M, Martini D, et al. Overview of human intervention studies evaluating the impact of the Mediterranean diet on markers of DNA damage. Nutrients. 2019;11(2). (PubMed)
121. Giacosa A, Barale R, Bavaresco L, et al. Cancer prevention in Europe: the Mediterranean diet as a protective choice. Eur J Cancer Prev. 2013;22(1):90-95. (PubMed)
122. Schwingshackl L, Schwedhelm C, Galbete C, Hoffmann G. Adherence to Mediterranean diet and risk of cancer: an updated systematic review and meta-analysis. Nutrients. 2017;9(10). (PubMed)
123. Ali Mohsenpour M, Fallah-Moshkani R, Ghiasvand R, et al. Adherence to Dietary Approaches to Stop Hypertension (DASH)-style diet and the risk of cancer: a systematic review and meta-analysis of cohort studies. J Am Coll Nutr. 2019;38(6):513-525. (PubMed)
124. Tabung FK, Brown LS, Fung TT. Dietary patterns and colorectal cancer risk: a review of 17 years of evidence (2000-2016). Curr Colorectal Cancer Rep. 2017;13(6):440-454. (PubMed)
125. Mohseni R, Mohseni F, Alizadeh S, Abbasi S. The association of Dietary Approaches to Stop Hypertension (DASH) diet with the risk of colorectal cancer: a meta-analysis of observational studies. Nutr Cancer. 2019:1-13. (PubMed)
126. Aune D, Chan DS, Lau R, et al. Dietary fibre, whole grains, and risk of colorectal cancer: systematic review and dose-response meta-analysis of prospective studies. BMJ. 2011;343:d6617. (PubMed)
127. Lu D, Pan C, Ye C, et al. Meta-analysis of soy consumption and gastrointestinal cancer risk. Sci Rep. 2017;7(1):4048. (PubMed)
128. Zhu B, Sun Y, Qi L, Zhong R, Miao X. Dietary legume consumption reduces risk of colorectal cancer: evidence from a meta-analysis of cohort studies. Sci Rep. 2015;5:8797. (PubMed)
129. Encarnacao JC, Abrantes AM, Pires AS, Botelho MF. Revisit dietary fiber on colorectal cancer: butyrate and its role on prevention and treatment. Cancer Metastasis Rev. 2015;34(3):465-478. (PubMed)
130. Chatterjee M, Roy K, Janarthan M, Das S, Chatterjee M. Biological activity of carotenoids: its implications in cancer risk and prevention. Curr Pharm Biotechnol. 2012;13(1):180-190. (PubMed)
131. Kumar S, Pandey AK. Chemistry and biological activities of flavonoids: an overview. Scientific World Journal. 2013;2013:162750. (PubMed)
132. Rauf A, Imran M, Butt MS, Nadeem M, Peters DG, Mubarak MS. Resveratrol as an anti-cancer agent: A review. Crit Rev Food Sci Nutr. 2018;58(9):1428-1447. (PubMed)
133. Vallianou NG, Evangelopoulos A, Schizas N, Kazazis C. Potential anticancer properties and mechanisms of action of curcumin. Anticancer Res. 2015;35(2):645-651. (PubMed)
134. Woyengo TA, Ramprasath VR, Jones PJ. Anticancer effects of phytosterols. Eur J Clin Nutr. 2009;63(7):813-820. (PubMed)
135. Wu X, Cheng J, Wang X. Dietary antioxidants: potential anticancer agents. Nutr Cancer. 2017;69(4):521-533. (PubMed)
136. Nabavi SF, Bilotto S, Russo GL, et al. Omega-3 polyunsaturated fatty acids and cancer: lessons learned from clinical trials. Cancer Metastasis Rev. 2015;34(3):359-380. (PubMed)
137. Wu L, Wang Z, Zhu J, Murad AL, Prokop LJ, Murad MH. Nut consumption and risk of cancer and type 2 diabetes: a systematic review and meta-analysis. Nutr Rev. 2015;73(7):409-425. (PubMed)
138. Hashemian M, Murphy G, Etemadi A, Dawsey SM, Liao LM, Abnet CC. Nut and peanut butter consumption and the risk of esophageal and gastric cancer subtypes. Am J Clin Nutr. 2017;106(3):858-864. (PubMed)
139. Nieuwenhuis L, van den Brandt PA. Tree nut, peanut, and peanut butter consumption and the risk of gastric and esophageal cancer subtypes: the Netherlands Cohort Study. Gastric Cancer. 2018;21(6):900-912. (PubMed)
140. Grosso G, Yang J, Marventano S, Micek A, Galvano F, Kales SN. Nut consumption on all-cause, cardiovascular, and cancer mortality risk: a systematic review and meta-analysis of epidemiologic studies. Am J Clin Nutr. 2015;101(4):783-793. (PubMed)
141. Fadelu T, Zhang S, Niedzwiecki D, et al. Nut consumption and survival in patients with stage III colon cancer: results from CALGB 89803 (Alliance). J Clin Oncol. 2018;36(11):1112-1120. (PubMed)
142. Pereira PM, Vicente AF. Meat nutritional composition and nutritive role in the human diet. Meat Sci. 2013;93(3):586-592. (PubMed)
143. Domingo JL, Nadal M. Carcinogenicity of consumption of red meat and processed meat: A review of scientific news since the IARC decision. Food Chem Toxicol. 2017;105:256-261. (PubMed)
144. Boada LD, Henriquez-Hernandez LA, Luzardo OP. The impact of red and processed meat consumption on cancer and other health outcomes: Epidemiological evidences. Food Chem Toxicol. 2016;92:236-244. (PubMed)
145. Demeyer D, Honikel K, De Smet S. The World Cancer Research Fund report 2007: A challenge for the meat processing industry. Meat Sci. 2008;80(4):953-959. (PubMed)
146. Carr PR, Walter V, Brenner H, Hoffmeister M. Meat subtypes and their association with colorectal cancer: Systematic review and meta-analysis. Int J Cancer. 2016;138(2):293-302. (PubMed)
147. Yi M, Wu X, Zhuang W, et al. Tea consumption and health outcomes: umbrella review of meta-analyses of observational studies in humans. Mol Nutr Food Res. 2019:e1900389. (PubMed)
148. Koo MW, Cho CH. Pharmacological effects of green tea on the gastrointestinal system. Eur J Pharmacol. 2004;500(1-3):177-185. (PubMed)
149. Zhang YF, Xu Q, Lu J, et al. Tea consumption and the incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Eur J Cancer Prev. 2015;24(4):353-362. (PubMed)
150. Chen Y, Wu Y, Du M, et al. An inverse association between tea consumption and colorectal cancer risk. Oncotarget. 2017;8(23):37367-37376. (PubMed)
151. Yuan JM. Cancer prevention by green tea: evidence from epidemiologic studies. Am J Clin Nutr. 2013;98(6 Suppl):1676s-1681s. (PubMed)
152. Andrici J, Eslick GD. Hot food and beverage consumption and the risk of esophageal cancer: a meta-analysis. Am J Prev Med. 2015;49(6):952-960. (PubMed)
153. Huang Y, Chen H, Zhou L, et al. Association between green tea intake and risk of gastric cancer: a systematic review and dose-response meta-analysis of observational studies. Public Health Nutr. 2017;20(17):3183-3192. (PubMed)
154. Fardet A. New hypotheses for the health-protective mechanisms of whole-grain cereals: what is beyond fibre? Nutr Res Rev. 2010;23(1):65-134. (PubMed)
155. Rampal S, Yang MH, Sung J, et al. Association between markers of glucose metabolism and risk of colorectal adenoma. Gastroenterology. 2014;147(1):78-87.e73. (PubMed)
156. Aune D, Keum N, Giovannucci E, et al. Whole grain consumption and risk of cardiovascular disease, cancer, and all cause and cause specific mortality: systematic review and dose-response meta-analysis of prospective studies. BMJ. 2016;353:i2716. (PubMed)
157. Benisi-Kohansal S, Saneei P, Salehi-Marzijarani M, Larijani B, Esmaillzadeh A. Whole-grain intake and mortality from all causes, cardiovascular disease, and cancer: a systematic review and dose-response meta-analysis of prospective cohort studies. Adv Nutr. 2016;7(6):1052-1065. (PubMed)
158. Wei H, Gao Z, Liang R, Li Z, Hao H, Liu X. Whole-grain consumption and the risk of all-cause, CVD and cancer mortality: a meta-analysis of prospective cohort studies. Br J Nutr. 2016;116(3):514-525. (PubMed)