Nutrition Research
-
Macronutrients
-
Micronutrients
-
Dietary Factors
Summary
The immune system is constantly working to protect the body from infection, injury, and disease. It relies on an adequate supply of nutrients for its baseline functions as well as for ramping up its activity when necessary. It is well established that malnutrition (protein-energy malnutrition and obesity) and deficiencies in one or more micronutrients (vitamins and nutritionally essential minerals) diminish immune function. In most instances, correcting the nutrient deficiency restores the affected immune functions. At a minimum, getting the recommended dietary allowance (RDA) for vitamin C and vitamin D is necessary for the immune system to function properly; there is some evidence that intakes above the current RDA for these vitamins may be of further benefit. Because supplementation with iron can have unwanted side effects in those with preexisting infections, especially malaria, routine iron supplementation should be accompanied by malaria detection and treatment strategies. The long-chain omega-3 fatty acids, eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), have potent anti-inflammatory effects, especially in individuals with chronic or acute inflammation.
Overview
The immune system protects the body against infection and disease. It is a complex system of organs, tissues, and cells located throughout the body.
The immune system must recognize foreign invaders and abnormal cells (Table 1) and distinguish them from the body’s healthy cells. Autoimmune diseases happen when the body mounts an immune response against its own tissues instead of a foreign invader. Allergies occur when an individual’s immune system reacts to substances in the environment that are tolerated by most people.
Table 1. The Immune System Responds to Foreign Invaders and Abnormal Cells
|
Foreign Invaders |
Abnormal Cells |
|
Viruses |
Cancer cells |
|
Bacteria |
|
|
Parasites |
|
|
Mold |
|
|
Allergens |
|
The immune response is split into two functional divisions: innate and acquired immunity.
(1) Innate immunity is the first line of defense against foreign invaders. Innate immunity involves immediate, nonspecific responses to pathogens.
(2) Acquired immunity (also called adaptive immunity) is the second line of defense against foreign invaders. Acquired immunity involves a complex, targeted response to a specific pathogen. Exposure to a pathogen stimulates the production of certain immune cells that mark the pathogen for destruction. Upon first exposure, it takes several days or weeks to develop the acquired immune response, but the involved immune cells "remember" the encounter and respond quickly upon subsequent exposure to the same pathogen.
The components of the innate and acquired immune systems communicate and work together to protect the body from infection and disease (Table 2).
Table 2. Functional Divisions and Components of the Immune Response
Innate Immunity
(general response to a pathogen) |
Acquired Immunity
(specific response to a pathogen) |
|
Barriers |
Cells |
Humoral Factors |
Cells |
Humoral Factors |
|
Physical: skin, mucous membranes |
Phagocytes: engulf and destroy |
Eicosanoids: regulate inflammation |
T lymphocytes: detect specific pathogens, secrete cytokines, and coordinate an immune response |
Antibodies: specialized proteins that mark a pathogen for destruction |
|
Chemical: acidic environment of the stomach |
Mast cells: cause inflammation & symptoms of allergy |
Cytokines: regulate inflammation |
B lymphocytes: produce antibodies against a specific pathogen |
|
Biological: gut microbiota |
Natural killer (NK) cells: release toxic chemicals |
Complement proteins: attach to and destroy bacteria; some cause inflammation |
Complement proteins: attach to and destroy pathogens marked by antibodies |
Key features of the immune response
(1) Inflammation - inflammation is a central feature of a normal immune response. Inflammation serves to facilitate the delivery of immune cells, chemical messengers, and antibodies to a site of injury or infection. However, inappropriate activation of inflammation or the inability to turn off inflammation can lead to tissue damage and the development of chronic disease (see the article on Inflammation).
(2) Respiratory (oxidative) burst - phagocytes are a type of immune cell that engulf and destroy invading organisms. To help destroy invaders, certain phagocytes called neutrophils produce a concentrated burst of reactive oxygen species (ROS), damaging substances that help kill invading organisms. As is the case with inflammation, the respiratory burst is part of the normal immune response, but prolonged and continuous exposure to ROS can be damaging to tissues and contribute to chronic disease.
(3) Proliferation - proliferation means an increase in the number or amount of something. The immune system is constantly producing cells, chemical messengers, and proteins to carry out its functions. When it encounters a foreign invader, it ramps up production to respond accordingly. This process, called proliferation, requires energy, building blocks, and cofactors to produce the many cells and substances needed to mount an effective immune response.
DEFINITIONS
Pathogen - a disease-causing organism
Innate immunity - immediate, nonspecific immune response to foreign invaders
Acquired immunity - also called adaptive immunity; a complex, specific immune response to a foreign invader; the immune cells "remember" the invader and respond quickly upon subsequent encounters
Humoral factors - substances that travel in body fluids
Phagocytes - immune cells that engulf and destroy foreign invaders
Cytokines - a diverse assortment of chemical messengers that help immune cells communicate
B lymphocytes (B cells) - immune cells that produce antibodies
Antibody - a specialized protein that recognizes and binds to foreign proteins or pathogens in order to neutralize them or mark them for destruction
T lymphocytes (T cells) - immune cells that detect specific pathogens and coordinate an immune response
Natural killer (NK) cells - immune cells that release toxic chemicals to help destroy foreign invaders
Eicosanoids - compounds made from 20-carbon long-chain polyunsaturated fatty acids; the term 'eicosanoid' includes many compounds that can either cause or prevent inflammation
Reactive oxygen species - highly unstable oxygen-containing compounds that react easily with nearby cellular structures, potentially causing damage
Autoimmune disease - occurs when the body mounts an immune response against its own tissues instead of a foreign pathogen
Proliferation - an increase in the number or amount of something
References
Nutrition Research
DEFINITIONS
Test tube (in vitro) experiment - a research experiment performed in a test tube, culture dish, or other artificial environment outside of a living organism; in vitro is a Latin phrase meaning in glass
Animal experiment - a research experiment performed in a laboratory animal; many different animal species are studied in the laboratory, including terrestrial (land), aquatic (water), and microscopic animals
Observational study - a human research study in which no experimental intervention or treatment is applied, and participants are simply observed over time
Randomized controlled trial - a human research study in which participants are assigned by chance alone to receive either an experimental agent (the treatment group) or a placebo (the control group)
Placebo - a chemically inactive substance
Long-chain Omega-3 Fatty Acids
What they do
General
-
Essential fatty acids are polyunsaturated fatty acids (PUFAs) that cannot be synthesized in the body and must come from the diet. PUFAs have several double bonds in their structure that give them complex shapes and influence their function.
-
Essential fatty acids are structural components of every cell in the body and are converted to compounds that influence inflammation and immunity.
-
There are two classes of essential fatty acids: omega-6 PUFAs and omega-3 PUFAs.
Immune-specific
-
Both omega-3 and omega-6 PUFAs, particularly the long-chain PUFAs, influence the immune response.
-
The long-chain omega-6 PUFA arachidonic acid (AA) and the long-chain omega-3 PUFAs eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) are incorporated into immune cell membranes, where they influence immune cell structure and function.
-
Omega-3 and omega-6 PUFAs give rise to a variety of eicosanoids and bioactive lipid mediators — chemical messengers that regulate inflammation and immune cell action.
What we know
-
EPA and DHA have an overall anti-inflammatory effect.
-
Increasing EPA and DHA consumption increases the EPA and DHA content of immune cell membranes, mainly by displacing AA and becoming the substrate for the enzymes that synthesize eicosanoids.
-
EPA- and DHA-derived eicosanoids are less potent inducers of inflammation than eicosanoids derived from AA.
-
EPA and DHA also give rise to anti-inflammatory compounds that "turn off" the inflammatory response.
-
In chronic inflammatory states (e.g., rheumatoid arthritis, atherosclerosis), EPA plus DHA supplements have been shown to reduce symptoms of rheumatoid arthritis and the risk of cardiac events.
-
The dose of EPA plus DHA that is optimal for immune function in healthy individuals is not yet established.
-
Ingestion of at least 500 mg/day of EPA plus DHA is recommended by the International Society for the Study of Fatty Acids and Lipids (ISSFAL) and several other professional organizations.
-
The Linus Pauling Institute recommends that generally healthy adults eat fish twice weekly, which provides approximately 500 mg/day of EPA plus DHA; for those who do not regularly consume fish, consider taking a two-gram fish oil supplement several times a week in consultation with a physician.
-
Higher daily intakes may be recommended for the treatment of specific disorders.
For references and more information, see the section on Dietary lipids in the in-depth article on Immunity.

Overnutrition and Obesity
What it is
General
-
Overnutrition is a form of malnutrition in which nutrients (most often energy) are supplied in excess of the body’s needs.
-
Obesity, a state of excess fat storage, is associated with an increased risk of a number of chronic diseases, including high blood pressure, type 2 diabetes mellitus, liver and gallbladder disease, osteoarthritis, sleep apnea, and certain cancers.
-
Central obesity, excessive accumulation of fat around the abdominal area, in particular is linked to inflammation, metabolic risk factors, and the development of chronic disease.
Immune-specific
-
Obesity is characterized by a state of chronic, low-grade, systemic inflammation and there is some data to suggest that there is also immunosuppression. The inflammation is believed to originate from adipose tissue (where body fat is stored), which secretes hormones and chemical messengers that trigger inflammation and influence immune cell activity.
-
Obesity is often accompanied by deficiencies in micronutrients that are essential for proper immune function.
What we know
-
Obese individuals may exhibit increased susceptibility to infection and poor wound healing.
For references and more information, see the section on Overnutrition and obesity in the in-depth article on Immunity.

Protein-energy Malnutrition (PEM)
What it is
General
-
PEM is the result of extreme deficiency of calories and/or protein in the diet.
-
Clinical conditions of severe PEM are termed marasmus (deficiency of both dietary protein and calories) and kwashiorkor (deficiency of dietary protein).
-
PEM is most common in developing nations, the elderly, hospitalized individuals, and those with chronic disease that interferes with nutrient absorption and utilization.
Immune-specific
-
Without protein and calories, all of the body’s essential functions suffer, including immune function. In PEM, there are insufficient building blocks and energy to make immune cells and immune factors that protect the body from infection and disease.
-
There is considerable data to suggest that PEM suppresses the functioning of the acquired immune system.
What we know
-
According to the World Health Organization, more than one-third of the world’s underprivileged, preschool-age children (80 percent living in Asia, 15 percent in Africa, and 5 percent in Latin America) are affected by PEM; this malnutrition stunts physical growth and mental development, with lasting effects into adulthood. PEM also drastically increases the risk of disease and death.
-
PEM increases the susceptibility to infection by adversely affecting nearly all aspects of acquired immunity.
-
PEM is usually accompanied by deficiencies in essential micronutrients required for proper immune function, especially vitamin A, vitamin B6, folate, vitamin E, zinc, iron, copper, and selenium.
-
Nutritional intervention can improve nutrient status, reduce the occurrence of disease, and increase survival in children and chronically ill patients with PEM.
For references and more information, see the section on Protein-energy malnutrition (PEM) in the in-depth article on Immunity.

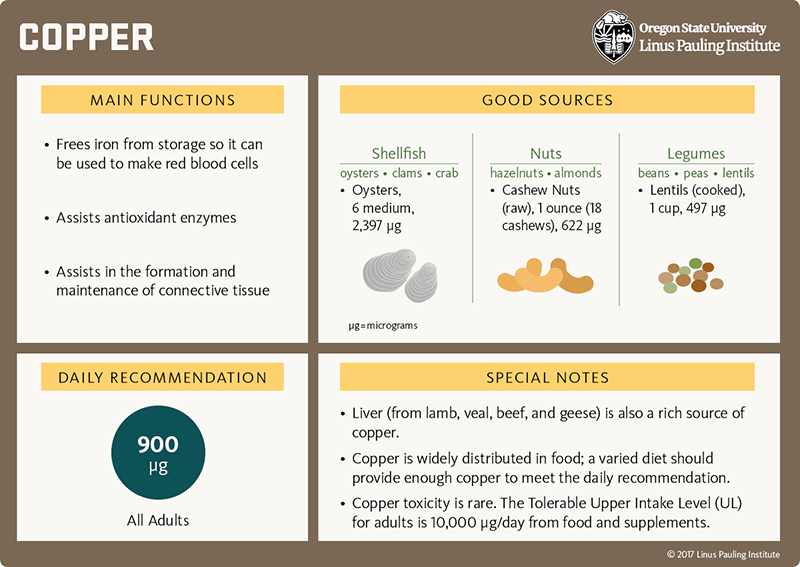
Copper
What it does
General
-
Copper is an essential mineral that assists in energy production, iron utilization, antioxidant defense, and the synthesis of neurotransmitters and connective tissue.
Immune-specific
-
Copper is a structural and functional component of an important antioxidant enzyme called superoxide dismutase that protects immune cells from oxidative damage.
-
Copper may also help cells of the innate immune response kill bacteria.
What we know
-
Severe copper deficiency results in neutropenia — an abnormally low number of immune cells called neutrophils; neutropenia can increase one’s susceptibility to infection.
-
On the other hand, long-term high intake of copper (7.8 milligrams/day for approximately five months) has been shown to blunt antibody production in response to an influenza vaccine.
-
Although extreme copper deficiency and excess can adversely affect immune function, it is very difficult to reliably measure copper nutritional status. Thus, the effect of marginal copper status on immune function is not yet known.
For references and more information, see the section on copper in the in-depth article on Immunity.
[Download PDF]

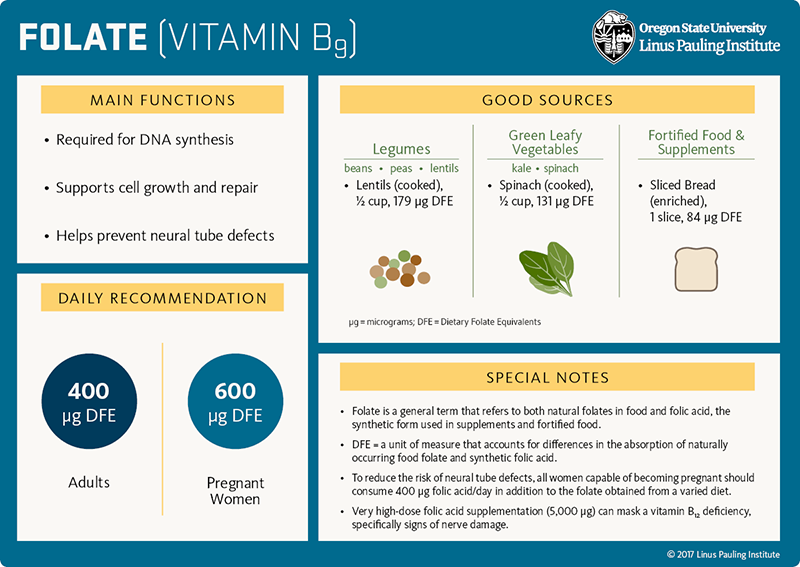
Folate
What it does
General
-
Folate is a B-vitamin required for DNA synthesis and the formation of new cells.
-
Additionally, the B-vitamins folate, vitamin B12, and vitamin B6 work together to convert homocysteine to methionine, an amino acid used in countless essential cellular activities.
Immune-specific
-
Because immune cells have high metabolic activity and high rates of proliferation, they require folate to form new immune cells and mount a proper immune response.
What we know
-
Animal studies and a few observational studies indicate that folate deficiency is associated with an increased susceptibility to infection.
-
In patients with severe folate deficiency, known as megaloblastic anemia, decreased numbers and activity of T lymphocytes have been observed.
-
Correcting the folate deficiency appears to restore the affected immune functions.
DEFINITION
Proliferation - an increase in the number or amount of something
For references and more information, see the section on folate in the in-depth article on Immunity.
[Download PDF]

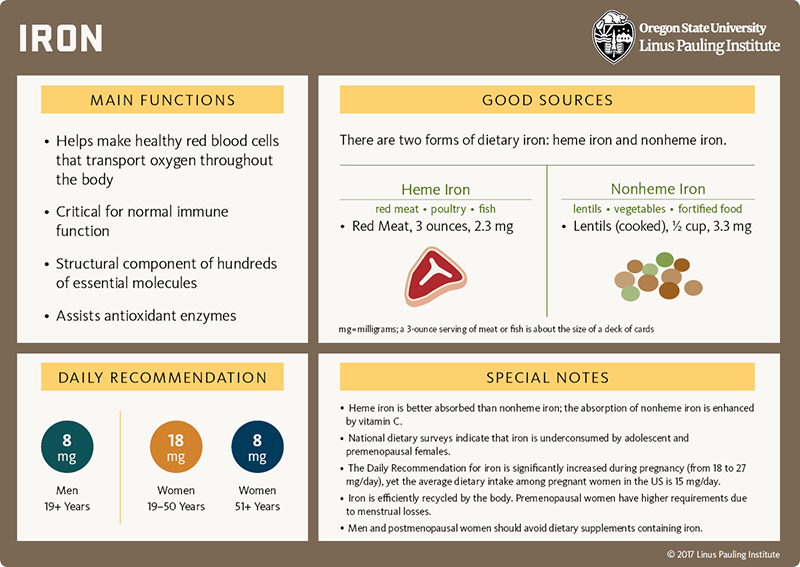
Iron
What it does
General
-
Iron, an essential mineral, helps make hundreds of vital proteins, facilitates oxygen transport and storage, participates in energy production, and assists antioxidant enzymes.
-
Dietary iron is found in two forms: heme and nonheme iron. Heme iron comes mainly from meat, poultry, and fish. Nonheme iron is found in plants, dairy products, meat, fortified food, and dietary supplements.
Immune-specific
-
Iron is a structural and functional component of several metabolic and antioxidant enzymes that are critical for normal immune function.
-
Sufficient iron is necessary for many immune functions, including the production of T lymphocytes and the generation of reactive oxygen species that kill pathogens.
-
Iron is also required by most infectious agents for replication and survival. The human body has developed strategies to withhold iron in response to infection or inflammation, but many infectious agents have developed their own counter measures to acquire iron while avoiding its toxic effects. Thus, a balance between host and pathogen iron requirements must be maintained for optimal immune function.
What we know
-
Both iron deficiency and iron overload are associated with impaired immune function and increased susceptibility to infection.
-
An estimated 30 percent of the world’s population (residing mainly in less developed nations) is iron deficient and correcting this deficiency is critically important for growth, development, immune function, survival, and quality of life. There is concern, however, that excess iron could increase the susceptibility to certain infections. In regions with high rates of malaria, combining iron administration with malaria detection and treatment strategies, and possibly screening for iron status, are important components of iron supplementation efforts.
-
Iron overload, studied mainly in individuals with genetic disorders of iron storage (hemochromatosis), has numerous negative effects on immune cell function and can make individuals especially vulnerable to pathogens.
HIGHLIGHT: IRON DEFICIENCY
-
Although iron deficiency is more common in developing nations, certain populations in the US are at risk for iron deficiency:
-
toddlers (ages 1 to 2 years) - approximately 7 percent are iron deficient
-
adolescent and adult females (ages 12 to 49 years) - 9 to 16 percent are iron deficient
-
pregnant females - 7 percent are iron deficient during the first trimester; 14 percent during the second trimester; and 30 percent during the third trimester
-
Adolescent and premenopausal females should increase consumption of foods rich in iron.
-
Most pregnant females will require iron supplements to meet the increased requirement during pregnancy (see the article on Pregnancy and Lactation).
-
The nutritional requirement for iron goes down with age. For men, postmenopausal women, and the elderly, supplemental iron is not recommended unless an individual has been diagnosed with iron deficiency.
Sources for statistics
-
Centers for Disease Control and Prevention (CDC). Morbidity Mortality Weekly Report. 2002 Oct 11;51(40):897-9
-
Mei Z, et al. Assessment of iron status in US pregnant women from the National Health and Nutrition Examination Survey (NHANES), 1999-2006. AJCN 2011;93:1312-20
DEFINITIONS
Antioxidant - a compound that prevents or repairs the damage caused by reactive oxygen species
Reactive oxygen species - highly unstable oxygen-containing compounds that react easily with nearby cellular structures, potentially causing damage
For references and more information, see the section on iron in the in-depth article on Immunity.
[Download PDF]

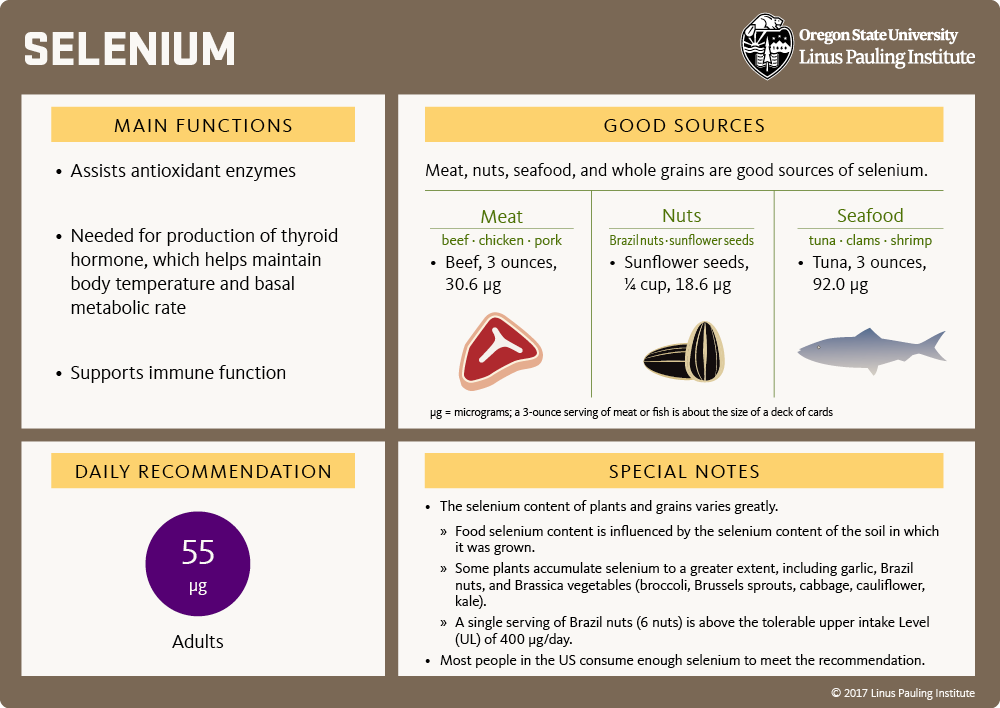
Selenium
What it does
General
-
Selenium is an essential trace mineral that is a structural component of several antioxidant enzymes and influences thyroid hormone function.
Immune-specific
-
Selenium is an integral component of two antioxidant enzymes, glutathione peroxidase and thioredoxin reductase, that protect immune cells from oxidative damage.
-
Selenium also influences the production of cytokines and eicosanoids — chemical messengers that regulate inflammation and immune cell function.
What we know
-
Selenium deficiency increases oxidative stress, which impairs immune function.
-
Selenium supplementation appears to improve some, but not all, immune functions:
-
Selenium supplementation improves the acquired immune response in selenium-deficient individuals and enhances the immune response to viruses.
-
On the other hand, selenium supplementation may worsen allergic asthma and impair the immune response to parasites.
-
Correcting a deficiency rather than supplementing selenium-adequate individuals may be best for optimal immune function.
For references and more information, see the section on selenium in the in-depth article on Immunity.
[Download PDF]

Vitamin A
What it does
General
-
Vitamin A (retinol) is a fat-soluble vitamin that is essential for normal vision, reproduction, cell growth and development, and immune function.
Immune-specific
-
Vitamin A helps maintain the integrity of the skin, eye, respiratory, gastrointestinal, and genitourinary tracts, thereby reinforcing our barriers against disease-causing organisms.
-
Vitamin A is required for the proper function of immune cells that generate antibodies. Good vitamin A status is essential for vaccines to work properly.
What we know
-
For children in developing nations, vitamin A deficiency causes severe visual impairment, blindness, and increases vulnerability and death from common childhood infections like measles and diarrheal disease.
-
In low- and middle-income countries, preventative vitamin A supplementation in children older than 6 months of age reduces the occurrence of diarrhea and measles and significantly improves child survival.
-
Because of potential adverse effects, vitamin A supplements should be reserved for undernourished populations and those with evidence of vitamin A deficiency.
For references and more information, see the section on vitamin A in the in-depth article on Immunity.

[Download PDF]

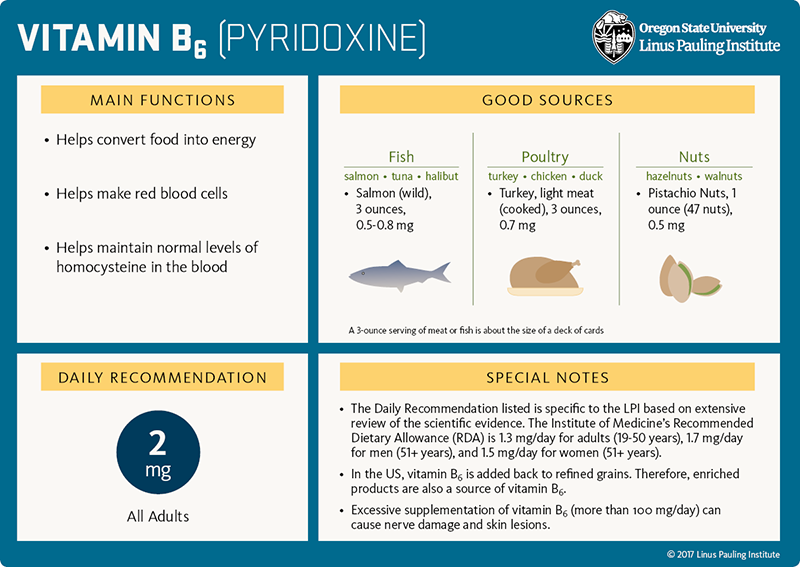
Vitamin B6
What it does
General
-
Vitamin B6 helps convert food into usable energy and assists in the formation of neurotransmitters, red blood cells, proteins, and DNA.
-
Additionally, the B-vitamins folate, vitamin B12, and vitamin B6 work together to convert homocysteine to methionine, an amino acid used in countless essential cellular activities.
Immune-specific
-
Because immune cells have high metabolic activity and high rates of proliferation, they require vitamin B6 to form new immune cells and mount a proper immune response.
What we know
-
Animal studies and a few, small randomized controlled trials indicate that vitamin B6 deficiency impairs immune function.
-
Specifically, several aspects of acquired immunity are reduced, such as lymphocyte production, antibody formation, and cytokine production.
-
Correcting the vitamin B6 deficiency appears to restore the affected immune functions.
DEFINITION
Proliferation - an increase in the number or amount of something
For references and more information, see the section on vitamin B6 in the in-depth article on Immunity.
[Download PDF]

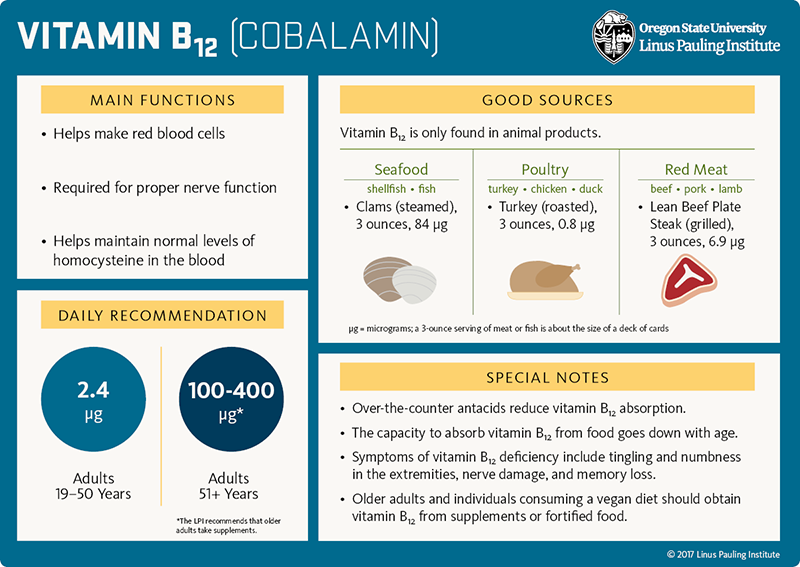
Vitamin B12
What it does
General
-
Vitamin B12 helps convert food into usable energy, is required for proper nerve function, and assists in the formation of red blood cells, proteins, and DNA.
-
Additionally, the B-vitamins folate, vitamin B12, and vitamin B6 work together to convert homocysteine to methionine, an amino acid used in countless essential cellular activities.
Immune-specific
-
Because immune cells have high metabolic activity and high rates of proliferation, they require vitamin B12 to form new immune cells and mount a proper immune response.
What we know
-
Severe vitamin B12 deficiency, known as pernicious anemia, suppresses natural killer cell activity and decreases numbers of circulating T lymphocytes.
-
Correcting the vitamin B12 deficiency appears to restore the affected immune functions.
DEFINITION
Proliferation - an increase in the number or amount of something
For references and more information, see the section on vitamin B12 in the in-depth article on Immunity.
[Download PDF]

Vitamin C
What it does
General
-
Vitamin C (ascorbic acid) is a water-soluble vitamin that neutralizes a variety of reactive oxygen species and recycles important cellular antioxidants.
-
Vitamin C is also a cofactor in numerous enzymatic reactions involved in the making of collagen, L-carnitine, and several neurotransmitters, and in the regulation of gene expression.
Immune-specific
-
Immune cells generate reactive oxygen species to kill invading organisms; vitamin C may protect immune and nearby cells from damage by these substances.
-
In vitro studies suggest that vitamin C may increase the production and function of certain immune cells that help engulf and kill foreign invaders.
What we know
-
Immune cells accumulate and concentrate vitamin C and then quickly use it up during an active immune response.
-
The scientific evidence regarding the effect of vitamin C supplementation on immune function is hampered by several methodological shortcomings. Important considerations for research studies on vitamin C and infections include:
-
the baseline vitamin C status of the study population. A beneficial effect of vitamin C supplementation on the immune system may occur only in those with low vitamin C intake and status to begin with.
-
the presence of modifying factors. Physical stress, oxidative stress, smoking, and disease may be accompanied by an increased demand for vitamin C.
-
At this time, the scientific evidence is insufficient to advocate vitamin C supplementation in the prevention of pneumonia in the general population.
-
Routine use of vitamin C supplements may have a mild, beneficial effect on the duration of the common cold in certain individuals.
DEFINITIONS
Reactive oxygen species - highly unstable oxygen-containing compounds that react easily with nearby cellular structures, potentially causing damage
Antioxidants - compounds that prevent or repair the damage caused by reactive oxygen species
In vitro experiment - a research experiment performed in a test tube, culture dish, or other artificial environment outside of a living organism; in vitro is a Latin phrase meaning in glass
Oxidative stress - a situation in which the production of reactive oxygen species exceeds the ability of an organism to eliminate or neutralize them
For references and more information, see the section on vitamin C in the in-depth article on Immunity.

[Download PDF]

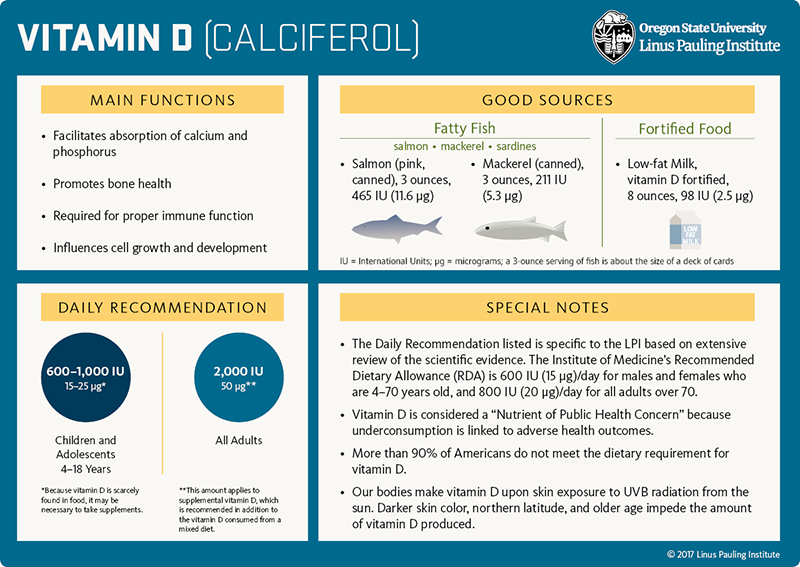
Vitamin D
What it does
General
-
Vitamin D is a fat-soluble vitamin that helps maintain calcium and phosphorus balance, promotes bone health, regulates immune function, and influences cell growth and development.
-
Vitamin D can be made in the skin (upon exposure to ultraviolet B [UVB] radiation from the sun) and obtained from dietary and supplemental sources.
Immune-specific
-
Vitamin D increases the expression of antimicrobial proteins.
-
Vitamin D limits certain aspects of the acquired immune response, playing a protective role and potentially reducing the risk of autoimmune disease and tissue transplant rejection.
What we know
-
Low serum 25-hydroxyvitamin D3 (a reliable measure of vitamin D status) is linked to a higher risk of upper respiratory tract infections.
-
Overall, randomized controlled trials indicate that daily or weekly supplementation with vitamin D reduces the risk of upper respiratory tract infections.
-
Vitamin D deficiency is associated with an increased incidence and severity of the coronavirus disease, COVID-19.
-
Low serum 25-hydroxyvitamin D3 has been observed in individuals with autoimmune disease, including those with insulin-dependent (type 1) diabetes mellitus, multiple sclerosis (MS), systemic lupus erythematosus, and rheumatoid arthritis. In those with MS, lower vitamin D status is associated with increased disease activity and risk of relapse.
-
Living at higher latitude (and thus, exposed to less UVB radiation from the sun) and low vitamin D intake have been associated with an increased risk of developing MS.
-
Despite the well-documented association between low vitamin D status and multiple autoimmune diseases, few randomized controlled trials have been conducted and the clinical efficacy of vitamin D supplementation in the prevention and treatment of autoimmune disease is not yet known.
HIGHLIGHT
-
Vitamin D is notoriously difficult to obtain from food sources alone and national surveys indicate that 94% of the US population is not meeting the dietary requirement for vitamin D.
-
The LPI recommends 2,000 IU (50 micrograms) of supplemental vitamin D daily for generally healthy adults.
For references and more information, see the sections on Acute respiratory infections and Coronavirus disease, COVID-19 in the vitamin D article, as well as the section on vitamin D in the in-depth article on Immunity.
[Download PDF]

Vitamin E
What it does
General
-
Vitamin E is a fat-soluble vitamin that functions as an antioxidant in lipid (fat) environments.
-
Vitamin E is an important antioxidant nutrient in cell membranes, where it functions to protect cells from oxidative damage.
Immune-specific
-
Vitamin E augments the functional activity of immune cells (T lymphocytes in particular) by protecting their cell membranes and reducing the production of immunosuppressive factors.
What we know
-
Several aspects of immune function decline with increasing age and older individuals are more susceptible to infection and have a poor response to vaccination.
-
Supplementation with vitamin E is able to reverse these deficits and enhance resistance to respiratory infection in some individuals.
-
However, the research in this area is still inconclusive; randomized controlled trials have reported positive, neutral, and negative effects of vitamin E supplementation on pneumonia and the common cold in certain subgroups of the population, including the elderly.
For references and more information, see the section on vitamin E in the in-depth article on Immunity.

[Download PDF]

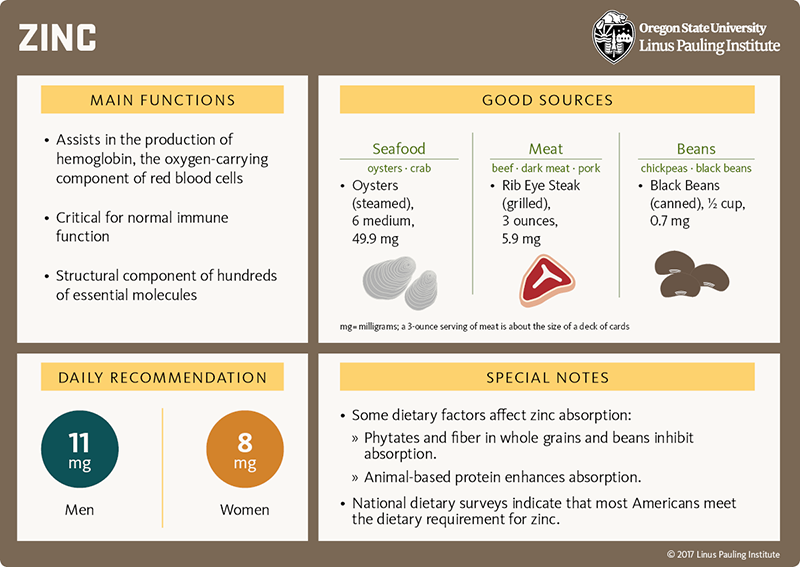
Zinc
What it does
General
-
Zinc is an essential trace mineral that is required for the synthesis of hundreds of essential proteins, needed for normal cell growth and development, facilitates oxygen transport and storage, and assists several antioxidant enzymes.
Immune-specific
-
Zinc is required for the growth and development of immune cells involved in both innate and acquired immunity.
-
Zinc is important for the synthesis of antibodies.
-
Zinc is also a structural and functional component of proteins and enzymes critical for normal immune function. One such zinc-containing antioxidant enzyme, superoxide dismutase, protects immune cells from reactive oxygen species that are generated to kill invading pathogens during an immune response.
What we know
-
Zinc deficiency is associated with an increased susceptibility to infection, especially in the elderly and children in developing countries.
-
Zinc supplementation (in combination with oral rehydration therapy) reduces the frequency, severity, and duration of diarrheal episodes in children.
-
The efficacy of zinc supplementation in elderly individuals is unclear at this time. Some randomized controlled trials have found that zinc supplementation reduces the number of infections, while others have found no effect.
-
Taking zinc lozenges upon the onset of common cold symptoms can reduce cold duration.
For references and more information, see the section on Impaired immune system function in the Zinc article.
[Download PDF]

Probiotics
What they are
General
-
Probiotics are live, beneficial bacteria that can be ingested and temporarily inhabit the lower part of the gastrointestinal tract (the colon).
-
The most commonly available probiotics are called Lactobacilli and Bifidobacteria. Sources of these probiotics include traditionally cultured dairy products, some fermented foods, and dietary supplements.
-
Because probiotics stay in the colon only temporarily, regular consumption is necessary to maintain their populations in the colon.
Immune-specific
-
The human body coexists with millions of bacterial species that can influence various aspects of health. The bacteria that live specifically in our colon (collectively referred to as the gut microbiota) can influence several aspects of immunity.
-
The gut microbiota influences immune function by: (1) creating a barrier against colonization by pathogens, and (2) interacting with host immune cells to influence their function.
-
The use of probiotics to influence immunity is an active area of research. Some ideas for how probiotics might help immunity are that they:
-
contribute to the maintenance of the antimicrobial barrier of the gut.
-
produce metabolic products, such as lactic acid and antibiotic proteins, that directly inhibit the growth of pathogens and influence the activity of host immune cells.
-
compete with some pathogenic bacteria for available nutrients.
What they do
-
Antibiotics can disrupt the protective barrier created by our gut microbiota. Probiotics have been shown to prevent diarrhea associated with antibiotic use in hospitalized children and adults.
-
At this time, the scientific evidence is insufficient to advocate the use of probiotics to reduce respiratory infections and improve vaccination response, especially in the elderly.
-
Probiotics facilitate the colonization of beneficial microbes in the colon.
For references and more information, see the section on Probiotics in the in-depth article on Immunity.

This content was underwritten, in part, by a grant from Bayer Consumer Care AG, Basel, Switzerland.